This woman is talking to me, maybe you. She talked about her shame in away I’m unable to articulate, she can see her failures in a light when I’m in the dark. Please watch the video, maybe she will touch your life too. Melinda
Month: November 2019
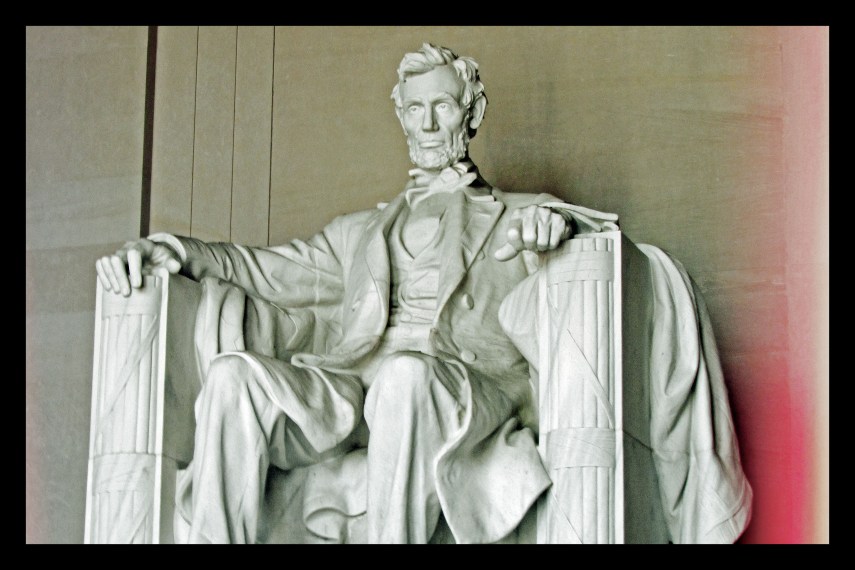
#Wordless Wednesday
Why Joker’s depiction of mental illness is dangerously misinformed
Annabel Driscoll and Mina Husain
The Guardian Mon 21 Oct 2019 11.04 EDT
With films playing a key role in shaping attitudes to mental health, two doctors say Joaquin Phoenix’s troubled supervillain perpetuates damaging stereotypes
As junior doctors who work on acute inpatient psychiatric wards, serious mental illness is our daily reality. We have, therefore, watched the controversies around Todd Phillips’s Joker – in which Joaquin Phoenix plays a troubled loner who turns to violence – with professional interest.
The film’s dominance in the debate about portrayals of mental illness in the movies comes at a curious time. Recently, we’ve witnessed great leaps of awareness about relatively common mental-health issues such as depression and anxiety, and with that awareness, increasing dismissal of the sort of unhelpful prejudices that used to surround them. These are now readily discussed without shame and often represented in the media with a well-informed grasp of the facts, thanks to effective information campaigns.
Joker review – the most disappointing film of the year
2 out of 5 stars. Read more
However, severe mental health conditions, such as psychotic illnesses, remain shrouded in stigma and are consistently misrepresented and misunderstood. Portrayals of mental illness in film can perpetuate unfounded stereotypes and spread misinformation. One of the more toxic ideas that Joker subscribes to is the hackneyed association between serious mental illness and extreme violence. The notion that mental deterioration necessarily leads to violence against others – implied by the juxtaposition of Phoenix’s character Arthur stopping his medication with his increasingly frequent acts of violence – is not only misinformed but further amplifies stigma and fear.
Studies show this association is exaggerated and people with severe mental illness are more vulnerable to violence from others than the general population. Interesting, then, that Joker’s earnest attempt to create an empathetic character with mental illness – who writes: “The worst part of having a mental illness is people expect you to behave as if you don’t” – contributes to the very prejudice that Arthur longs to evade.
Arthur’s supposed loss of grip on reality is suggested by a peppering of nods to psychotic symptoms: delusional ideas of a grandiose nature (“I am an undiscovered comedic genius”) and hallucinations of his neighbour – which are confirmed by his eventual admission to a psychiatric institution. This restoration of order via Arkham Asylum affirms the overarching inference of
the film: Arthur’s descent into violence and destruction is triggered by his mental deterioration. The result of this is to – disappointingly – remove Arthur’s agency and divert attention from a potentially more stimulating conversation about wealth inequality and its responsibility for societal collapse.
We wouldn’t want to get bogged down in labels, but the psychopathology Arthur inhabits is foggy at best: his apparent lack of disordered thinking means the attempt to illustrate psychosis is half formed. He also displays traits of narcissism and depression. This diagnostic vagueness may create a more relatable character that reflects the pain of any psychiatric illness; but it gives the impression that many disorders have been squashed into a plot device. In the end, it undermines Phoenix’s hypnotic performance and Joker’s sincere attempts to explore the interaction between poverty, inequality and social isolation.

Joker – the incels, the incitement, the ending: discuss with spoilers
Read more
Arthur’s chilling quirk – his bursts of incongruous and uncontrolled laughter – is no laughing matter either. Presumably, he suffers from the neurological condition pseudobulbar affect – also known as “emotional incontinence” – perhaps caused by his childhood head trauma. Joker may make an attempt to unpick the difference between the psychiatric and the neurological – between a mental illness and a medical disorder – but it runs the risk of conflating the two with a haunting, stigmatising and problematic image. Whether intentionally or not, Arthur comes across as a hysterically laughing supervillain, stereotypically “mad” to the untrained eye; a murderous clown laughing alone on a bus.
Cinematic depictions of mental illness – most infamously, One Flew Over the Cuckoo’s Nest – have profound and lasting implications in the real world. It is widely acknowledged within psychiatry that Cuckoo’s Nest led to inappropriate levels of suspicion and misinformation regarding electro-convulsive therapy, and may have meant many people did not receive treatment that is proved and effective. All this due to a single film’s misinformed presentation.
Films have the power to perpetuate stigma and fear, which is why the misrepresentation of severe mental illness in Joker should not be dismissed lightly.
On My Bookshelf: Mayo Clinic Guide to Fibromyalgia — Guest Blogger Reclaiming HOPE

When you first got your diagnosis of fibromyalgia, did you ever wish you had a guidebook to help you find your way through this ‘new
On My Bookshelf: Mayo Clinic Guide to Fibromyalgia — Reclaiming HOPE
U.S. PAIN FOUNDATION SUBMITS COMMENTS TO CMS RFI
October 16, 2019/ U.S. Pain Foundation/ 0 Comments
October 11, 2019
Centers for Medicare & Medicaid Services (CMS)
Comments on the Request for Information (RFI) on the Development of a CMS Action Plan to Prevent Opioid Addiction and Enhance Access to Medication-Assisted Treatment
The U.S. Pain Foundation is pleased to respond to CMS’s request for information to inform the development of a CMS Action plan to prevent opioid addiction and improve the treatment of acute and chronic pain. The U.S. Pain Foundation is the largest 501 (c) (3) organization for people who live with chronic pain from a myriad of diseases, conditions and serious injuries. Our mission is to connect, support, educate and advocate for those living with chronic pain, as well as their caregivers and healthcare providers.
Chronic pain is an enormous public health problem. The CDC and NIH have reported that 50 million Americans live with chronic pain and 19.6 million live with high-impact chronic pain that interferes with their ability to
1
There are currently very few highly effective treatments for many pain conditions. Managing pain is a matter of finding the right combination of treatments that allows pain sufferers to function and have some quality of life. We believe people with chronic pain should have access to a wide range of therapies and treatments because pain is very individual – what helps one person living with pain will not necessarily help another.
Most people living with chronic pain spend years of trial and error searching for treatments that will help to reduce their pain, while struggling to manage their lives. This is extremely wasteful from a personal standpoint as well as an economic one.
We believe that when it comes to chronic pain, CMS’s goal should be to get beneficiaries effective treatment sooner. Our recommendations for accomplishing this are as follows:
1. Compensate physicians for time spent coordinating complex care
Chronic pain patients require more time from their health care providers, because by its very nature, chronic pain is complex and challenging to treat. Doctors should be able to spend more time conducting a thorough pain assessment and developing a treatment plan at the first visit rather than
1 CDC. Prevalence of Chronic Pain and High Impact Chronic Pain Among Adult – U.S., 2016. MMWR Rep 2018;67:1001-6.
contact@uspainfoundation.org Main: (800) 910.2462 670 Newfield Street, Suite B 1 http://www.uspainfoundation.org Fax: (800) 929 -4062 Middletown, CT 06457
function on a daily basis.
with chronic pain and 5.4 million live with high-impact chronic pain. The Medicare population also includes disabled Americans younger than 65. Since pain is the number one cause of disability in the U.S., we can therefore assume that the number of Medicare beneficiaries living with pain is much higher than those reported numbers. Because many Americans living with high-impact chronic pain are unable to work or can only work part-time, many also depend on Medicaid.
That same study reported that of Americans over the age of 65, 13.5 million live
the fifth visit to the fifth doctor which is the current norm. Furthermore, because the cause, manifestations, and severity of chronic pain can vary so widely from person to person, there is no simple or uniform solution to managing it. Each patient is entirely unique and requires a unique treatment plan.
Individualized, multimodal, integrative care is widely understood to be the best and most effective approach to managing pain. But it requires time and resources to identify and try various modalities and coordinate this care. A traditional 10-minute appointment does not provide sufficient time for a provider to create and implement a multimodal treatment plan, and to continually reassess that plan as the individual’s health and pain change over time.
The lack of reimbursement for coordinating care and managing complex care is perhaps one of the most significant impediments to proper pain care. It has resulted in an overuse of quick fixes—like a reliance on medication alone.
- Reimburse for multimodal, multidisciplinary treatmentRehabilitation models of care, which emphasize integrated, multi-modal treatment, have been proven to be the most effective in reducing pain and improving function. Too often, pain management attempts to put a mere band-aid on pain levels, rather than address pain’s effects on function and quality of life. Chronic pain is a biopsychosocial disease, meaning it affects every aspect of an individual’s life, even more so when the individual lives with high-impact chronic pain. Thus, patients need and deserve care that addresses pain at multiple levels. For example, while medication and injections may help control pain, they do not give individuals tools for learning to live within their limitations. Restorative and complementary therapies, like physical therapy, occupational therapy, massage, yoga, and so on, are more suited to improving function and productivity and learning to live day-to-day with painful symptoms. Meanwhile, it is well-known that anxiety, depression, and other mental health conditions are common comorbidities of long-term pain. In fact, recent numbers from the CDC demonstrated that at least 10 percent of suicides in America involve someone living with pain. This vulnerable population needs earlier multimodal intervention that recognizes the full impact of pain on a person’s life. Patients with pain—especially those with high-impact pain—should have access to psychosocial care, including psychological counseling and peer support groups that is tailored to their unique challenges.Unfortunately, we have moved away from a bundled payment approach to this type of care, to the detriment of people with pain. It’s vital we return to reimbursing for multimodal, multidisciplinary treatment..
- Incentivize innovative value-based models of care that integrate multimodal treatmentThe cardiac care model, which incorporates exercise, nutrition and other modalities, is one innovative
contact@uspainfoundation.org Main: (800) 910.2462 670 Newfield Street, Suite B 2 http://www.uspainfoundation.org Fax: (800) 929 -4062 Middletown, CT 06457
approach that has been very successful and cost-effective at reducing the burden of heart disease. This is a model that takes into account that heart disease must be attacked from multiple angles, and that treatments and therapies work best in combination with one another.
This model also has proven that multidisciplinary, multimodal care can be cost-effective care. By investing health care dollars up front in managing heart disease and preventing cardiac events, we have saved millions of dollars in terms of reducing hospitalizations and emergency room visits. Beyond saving on direct healthcare costs, no price tag can account for the enormous reduction in suffering and lives lost.
Chronic pain is just as complex as heart disease. It similarly gets worse—and more expensive to treat– without comprehensive, multimodal early intervention. CMS should encourage and reimburse innovative integrated models of care for chronic pain.
- Remove access barriers to evidence-based non-opioid drugs and medical devicesCMS should require that at least two medications in each class of non-opioid medications commonly used for pain—such as antidepressants (SSRIs, SNRIs, or tricyclics), anticonvulsants, corticosteroids, NSAIDs, muscle relaxers, triptans, calcium channel blockers, topicals and so on)—are in the lowest-cost tier in every Part D plan formulary.It is vital to recognize that, again, each individual is unique, and what works for one person may not work for another. Patients must have access to various options to determine what reduces their pain levels. Unfortunately, many patients cannot afford the high copays on these medications, creating enormous and unnecessary barriers to safer, non-opioid medications. If CMS is committed to reducing opioid use, it must make alternative medications more affordable.In addition, an increasing number of evidence-based medical devices for pain management are available, with more coming to market each year. These devices represent an important category of treatment, especially in that they often provide sustained relief and generally come with less side effects than many other interventions. CMS must work to improve access to these types of devices by reducing out-of-pocket costs and removing overburdensome prior authorization requirements. In particular, CMS should remove the requirement for a psychological evaluation prior to obtaining spinal cord stimulation devices. There is no such requirement for surgery, which is much riskier, or for other treatments for pain.
- Partner with NIH/NCCIH to continue to build the evidence base for complimentary treatments like acupuncture for chronic low back pain (ie. therapeutic massage, yoga, tai chi, aquatherapy)
This is an area where data collection is essential to determining the value of these modalities for pain control. There is much anecdotal evidence that many complimentary techniques, especially gentle
contact@uspainfoundation.org Main: (800) 910.2462 670 Newfield Street, Suite B 3 http://www.uspainfoundation.org Fax: (800) 929 -4062 Middletown, CT 06457
exercise and mobility programs, are helpful in the ongoing management of chronic pain. These interventions can also be cost-effective, especially those that train patients on a program they can then practice at home. Exercise and mobility programs also do a lot to restore function, in addition to general pain reduction. But there is a lack of funding to do the randomized control trials that are necessary to prove their value. If we are truly committed to reducing opioid use, we must investigate and make available evidence-based alternatives for pain relief.
- Reimburse for promising treatments in specific conditions as evidence becomes available.The approach that CMS is using for chronic low back pain and acupuncture is an excellent model. In this instance, CMS is focusing on a narrow pain condition with one modality and a large subject population. This approach correctly recognizes that different modalities work differently for different types of pain—and must be studied accordingly. In particular, we commend CMS for covering treatment costs as part of this study. This reflects an understanding that cost is an enormous barrier to care, especially for the Medicare and Medicaid populations, who typically have limited ability to work. We would recommend using this approach simultaneously for other specific conditions.
- Encourage states to make more complementary and integrative care available through MedicaidA number of states have granted Medicaid waivers to cover complementary treatment for specific pain conditions and then studied the effect of these modalities on patients’ pain levels and function. One such example we are aware of is a waiver in Colorado to cover complementary treatments for spinal cord injury. We urge CMS to support more states in offering this type of Medicaid coverage.
- Incentivize participation in pain management group programs, similar to Medicare Silver Sneaker Program for fitness club membership & Medicare’s Diabetes Prevention Program
These programs have proven track records of helping patients more effectively cope with and manage chronic illness. Educating patients about ways to engage in self-management of their condition, and then incentivizing such self-care, could have a similarly positive impact on the pain population. If patients were reimbursed for the cost of membership in these programs, it would help them maintain wellness and function. - Reimburse for participation in chronic pain-specific patient education self-management and support group programs
Similar to above, patient education on self-management and coping skills are key to living successfully with a chronic condition. These programs can be taught via support group models and provide essential information on topics such as: cognitive behavioral therapy; stress reduction techniques, like meditation; strategies for activity restriction and modification; and much more.Isolation, stigma, and a sense of helplessness are enormous problems faced by the pain population,and create significant barriers to care. As mentioned before, people with chronic pain have
contact@uspainfoundation.org Main: (800) 910.2462 670 Newfield Street, Suite B 4 http://www.uspainfoundation.org Fax: (800) 929 -4062 Middletown, CT 06457
significantly higher incidences of mental health comorbidities, and are at greater risk of suicide.
It is well-known that mood disorders and stress can increase pain levels, and vice versa, creating a vicious cycle. CMS has a vested interest in providing more comprehensive care, that treats the whole patient—mind and body. Creating opportunities for connection, community, and education is vitally important.
10. Begin a serious effort to code for, collect, and analyze data on chronic pain in the Medicare and Medicaid population
CMS does not collect nor analyze epidemiologic data on chronic pain in its beneficiaries. We do not know the incidence of chronic pain in general, the prevalence of various pain conditions, trends over time, subpopulations at risk, nor the health consequences of pain in terms of morbidity, mortality and disability. It is critical to have this data to understand the scope of the problem. It is also vital in order to assess whether the improvements in care and interventions CMS undertakes in the Action Plan are effective in reducing the enormous burden of chronic pain.
In Section 6032 of the SUPPORT Act, Congress has called on CMS to use its authority to improve access to care for the millions of Americans whose lives have been devastated by the dual public health crises of opioid use disorder and pain. We are hopeful that CMS will give serious consideration to the recommendations we and others, such as the HHS Pain Management Best Practices Task Force have proposed. Now is the time for CMS to take bold and innovative action to ameliorate the enormous burden of chronic pain in America.
Sincerely,
Cindy Steinberg
National Director of Policy & Advocacy U.S. Pain Foundation
781-652-0146 cindy@uspainfoundation.org
contact@uspainfoundation.org Main: (800) 910.2462 http://www.uspainfoundation.org Fax: (800) 929 -4062
670 Newfield Street, Suite B 5 Middletown, CT 06457
INTERIM CEO A KEYNOTE SPEAKER AT AMERICAN MASSAGE THERAPY ASSOCIATION CONVENTION
October 31, 2019/ U.S. Pain Foundation/ 0 Comments
Interim CEO Nicole Hemmenway was one of three keynote speakers at the closing session of the American Massage Therapy Association (AMTA) national convention last weekend in Indianapolis, IN.
In her talk, “Massage for Chronic Pain: What our community wants you to know,” Hemmenway shared her personal journey with complex regional pain syndrome and why she’s dedicated herself to helping others with pain through the U.S. Pain Foundation. She gave attendees a glimpse into the programs and services U.S. Pain offers, and provided insight into the scope of the chronic pain health crisis in America.
The emphasis of Hemmenway’s remarks was on the barriers to multidisciplinary care, particularly massage, and how massage therapists can best help people with pain.
“It truly was a privilege to be invited by the AMTA to speak at their annual convention,” Hemmenway says. “There is a greater need, maybe now more than ever, for affordable access to multidisciplinary care, such as massage therapy. I was so impressed with the therapists I spoke to who are genuinely invested in patient’s overall wellness. But like the pain community, they also feel discouraged by the lack of access. That is why it is so important for us to use our voices to fight for better coverage of options like massage.”
Hemmenway shared feedback from the pain community about what they wanted massage therapists to know, including:
- People with pain have bodies that are very sensitive and complex. Pain continually evolves and changes, which means communication is vital to ensure that the massage is beneficial and to avoid making the pain worse.
- Maintaining a baseline can be just as important as achieving improvement (sometimes improvement isn’t possible); setting realistic goals is necessary.
- Massage therapy can be an important treatment option, but barriers exist, namely cost and transportation. Massage therapists should take into consideration things like providing more flexible pricing packages, offering in-home massages for those who are homebound, etc.
To learn more about U.S. Pain’s recent efforts related to complementary therapies, click here.
Women: 90% More Right Than Men — Guest Blogger The Alchemist’s Studio

Our raku pottery vase today, ‘Tiresias’ Prophecy’ tells the tale of blind creation, an ancient oracle, an instant gender reassignment, a spat between gods, and a lesson all men should be sure to take heed of – the woman is always right. 557 more words
Women: 90% More Right Than Men — The Alchemist’s Studio
It isn’t easy being president
Thanks for your thoughts Linda
#SoCS Prompt “nuts”

Your Friday prompt for Stream of Consciousness Saturday is “nuts.” Use it any way you’d like. Have fun!
This is an easy prompt because I’ve been called nuts many times in my life and I love nuts. Let’s start with why someone would call me nuts. I was and still am a tomboy and would do any dare or anything to keep up with the boys when I was younger. We played football, had a bike ramp, used the city culverts as bike ramps and I can’t forget the nutty games we played in the pool. I don’t feel the need to compete with boys/men today but still am a tomboy. Noone is going to limit what I can do or learn.
Growing up my grandparents had these 100 year old pecan trees and finding plenty of nuts was never a problem. When I was little gramps and I would collect off the nuts off the ground and sit in lawn chairs cracking, eating and feeding some to the squirells. Gramps reached a point where the squirells would come right up and take a nut out of his hand. I was able to do it one time but as cute as squirells are they carry rabies and I don’t want to find out. I could talk about nuts all day because of gramps, he never went a day without eating pecans, usually grow in the back yard.
Have a great weekend. Thanks for reading, I appreciate you and your awesome comments.
Melinda
Here are the rules:
- Your post must be Stream of Consciousness writing, meaning no editing (typos can be fixed), and minimal planning on what you’re going to write.
- Your post can be as long or as short as you want it to be. One sentence – one thousand words. Fact, fiction, poetry – it doesn’t matter. Just let the words carry you along until you’re ready to stop.
- I will post the prompt here on my blog every Friday, along with a reminder for you to join in. The prompt will be one random thing, but it will not be a subject. For instance, I will not say “Write about dogs”; the prompt will be more like, “Make your first sentence a question,” “Begin with the word ‘The,’” or will simply be a single word to get you started.
- Ping back! It’s important, so that I and other people can come and read your post! For example, in your post you can write “This post is part of SoCS:” and then copy and paste the URL found in your address bar at the top of this post into yours. Your link will show up in my comments for everyone to see. The most recent pingbacks will be found at the top. NOTE: Pingbacks only work from WordPress sites. If you’re self-hosted or are participating from another host, such as Blogger, please leave a link to your post in the comments below. https://lindaghill.com
- Read at least one other person’s blog who has linked back their post. Even better, read all of them! If you’re the first person to link back, you can check back later or go to the previous week by following my category, “Stream of Consciousness Saturday,” which you’ll find below the “Like” button on my post.
- Copy and paste the rules (if you’d like to) in your post. The more people who join in, the more new bloggers you’ll meet and the bigger your community will get!
- As a suggestion, tag your post “SoCS” and/or “#SoCS” for more exposure and more views.
- Have fun!
Sadfishing: Social media trend threatens teenagers’ mental health, report warns
Pupils seeking support online are being affected by latest trend
Education Correspondent
Tuesday 1 October 2019 07:38
A new social media trend called “sadfishing” is threatening teenagers’ mental health, report finds.
Youngsters facing genuine distress who seek support online are being accused of jumping onto the same publicity bandwagon as celebrities, according to research commissioned by headteachers.
“Sadfishing” has been used to describe when someone posts about an emotional problem in an attempt to attract attention, sympathy or hook an audience.
The term was coined after a number of celebrities, such as Kendall Jenner, were accused of teasing details about personal issues on their social media sites to drum up publicity and attract more likes.
A new study, by Digital Awareness UK (DAUK), says sadfishing is among the new trends that damage teenagers’ self-esteem, with teenagers reporting that they have been bullied as a result.
The report, which is based on face-to-face sessions with more than 50,000 pupils aged 11 to 16, argues that students can be left feeling disappointed at not getting the support they desire and it can subsequently make their emotional or mental health problems worse.
One Year 7 student told researchers that he used Instagram to share his feelings when he was feeling down due to problems at home.
“I got a lot of people commenting on and ‘liking’ my post but then some people said I was sadfishing the next day at school for attention,” the student said.
“Sharing my feelings online has made me feel worse in some ways but supported in others.”
There are also concerns that youngsters could be left vulnerable to online groomers, who prey on them by providing sympathy in order to gain their trust.
The report says: “DAUK is concerned about the number of students who are bullied for sadfishing (through comments on social media, on messaging apps or face-to-face), thus exacerbating what could be a serious mental health problem,”.
“We have noticed that students are often left feeling disappointed by not getting the support they need online.
“Groomers can also use comments that express a need for emotional support as a platform to connect with young people and gain their trust, only to try and exploit it at a later point.”
It goes on to give a case study of a teenage girl who had started a relationship with someone she met on social media through a mutual friend, after sharing her experiences of depression online.
He had responded to her post and shared his own experiences.
The young girl ended the relationship when she discovered he was much older than he claimed and he was pressurising her into sharing explicit images of herself.
Despite these negative findings, the report does also note that youngsters are becoming more tech-savvy and are more likely to manage their own use of technology responsibly.
The study was commissioned by the Headmasters’ and Headmistresses’ Conference (HMC) – a group of headteachers from some of the most prestigious private schools in the UK.
Chris Jeffery, chairman of the HMC wellbeing working group and headmaster of Bootham School in North Yorkshire, said: “It is encouraging to read of the growing signs of increased control that many young people are taking over their use of technology, but it is also helpful to know new ways in which it is proving to be a burden for them as .”
Charlotte Robertson, co-founder of DAUK, said: “Over the last year we’ve seen the digital landscape evolve at such rapid pace – particularly when it comes to the prevalence of data misuse, access to anonymous platforms and increased sharing of upsetting content.
“This has left many parents feeling overwhelmed by how best to empower their children to navigate the online world safely.”
#Weekend Music Share

I’m so glad you stopped by today. I appreciate you and so glad to be a part of your day. Melinda
Friday Quote




