There are many activities I can lose myself into, like photography, ancestry, looking at old photos of my family and ancestors, working in my garden, watching birds and researching topics of interest.
Melinda
There are many activities I can lose myself into, like photography, ancestry, looking at old photos of my family and ancestors, working in my garden, watching birds and researching topics of interest.
Melinda
I’m glad you joined me on Wordless Wednesday and I hope to see you soon.

Melinda
Back pain is one of the most common medical conditions, affecting millions of people around the world.
But did you know that apart from physical triggers (like pulling a muscle or slipping a disc), back pain can be caused or worsened by stress? Back pain and stress have a complex relationship that can flow both ways.
Evidence suggests that chronic stress can lead to chronic pain and vice versa. For many people, this involves back pain.
According to a 2021 study, chronic stress eventually leads to cortisol dysfunction as well as problems with the body’s inflammatory response. Cortisol and inflammation problems lead to oxidative stress, free radical damage, cellular injury or aging, and tissue degeneration, all of which can lead to chronic pain.
In addition, research has shown that stress has a direct effect on pain processing.
Overall, stress can be linked to back pain in several ways:
An analysis of 8,473 people found that severe stress was linked to a 2.8-fold increased risk of chronic low back pain compared to the general population. Another study of 77 police investigators found that stress was significantly linked to upper musculoskeletal pain. However, this particular study didn’t find a link between stress and lower back pain.
Stress-induced back pain varies from person to person and may show up differently, depending on its location.
Lower back pain is often characterized by a dull or sharp ache, stiffness, or muscle spasms, and it may also radiate to the legs or buttocks.
In contrast, upper back pain may cause a burning or stabbing sensation or a feeling of tightness or pressure between the shoulder blades. In some cases, upper back pain can also cause pain in the arms or chest.
It can be challenging to determine whether back pain is specifically caused by stress since back pain can have many different causes. However, here are some signs that may suggest that your back pain is stress-related:
The duration of stress-related back pain may vary depending on several factors. In some cases, it can go away on its own within a few days or weeks. However, if the underlying stress is not addressed, the pain may persist or worsen over time.
Some research suggests that stress can predict the presence of back pain later on. A study of 588 people found that, within a 2-year follow-up, the following stress types were identified as risk factors for back pain intensity and disability:
There are several things you can do to reduce stress-induced back pain, including:
Here are some tips for stress relief:
Stress and back pain are two interconnected conditions that can significantly impact your quality of life. Regular exercise, stretching, and good posture can help alleviate back pain, while stress management techniques like meditation and deep breathing can help reduce stress levels.
If you’re living with stress-related back pain, seek the help of a healthcare professional, such as a physical therapist or a counselor, who can provide valuable guidance and support in managing these issues.
Melinda
In this fast-paced social media world, it can be difficult to find the time to look within or back in time. I hope you find these quotes or questions interesting. I’m so glad you stopped by today!

Melinda
These shower steamers are great for self-care and make great gifts. I’ve looked on Amazon and was surprised by how expensive Steamers are. Treat yourself, your friends, and to family to these favorite shower steamers.
1 cup baking soda
1/2 cup citric acid
1/3 cup arrowroot powder
1/4 cup kaolin clay
Bowl: Large non-metallic
Spray the bottle with water
Nitrile gloves
Silicone mold: cylinder
45 drops of rosemary essential oil
45 drops peppermint essential oil
30 drops of chamomile essential oil
Dried leaves/herbs (optional)
150 drops of eucalyptus essential oil
Dried eucalyptus leaves, crushed (optional)
Mica: green (optional)
120 drops of peppermint essential oil
2 TB. menthol crystals Mica: Agua (optional)
Add all the dry ingredients to a large, non-metallic bowl and whisk until blended. Drop the essential oils on the dry ingredients, and stir to combine. The essential oils can create droplets, which will dissolve in the following step.
Spray the mixture with a little water and incorporate it immediately to avoid a reaction. If you don’t have a spray bottle, sprinkle water on the mixture using a teaspoon.
Put on nitrile gloves to protect your hands when kneading the mixture as the citric acid can irritate sensitive skin and nail polish. The mixture should feel like damp sand and be wet enough to hold its shape when pressed together. If using colored mica and dried herbs or flowers, add them to the mixture.
Fill the silicone mold with the mixture, and press firmly into the mold using your fingertips, paying attention to the edges. Let the mixture dry for 24-48 hours. Making shower steamers can be affected by the humidity; in a humid environment, the drying time may be longer. When they feel hard and solid, carefully peel back the mold and gently pop out of the disk. Store the steamers in an airtight container or jar, and ensure that the steamers aren’t exposed to water or moisture. The shelf life is one year.
Before use, let warm water run for several minutes to moisturize the air. It’s best to place the steamer away from the running water and the drain. Ideally, only the bottom of the tabs should be wet. You can also put a shower steamer in a soap dish. Breathe in deeply as the essential oils vaporize.
These are a year-round self-care treat. Make a huge batch and then you have some for gifts. Don’t forget your self-care, save some for yourself.
Melinda
God loves me
Jesus died for my sins
Artificial Intelligence is good and very bad
Climate change is real
My dogs love me
My husband loves me
Writing is the perfect outlet
My Grandparents past the through the pearly gates
Compromise is the start to finding a solution
The politics of today will change in future
I’m not sure what picture someone will draw about me after reading this post, I’d love your feedback.
Melinda
Gabapentin isn’t a narcotic or federally controlled substance, but it is regulated and recognized as a controlled substance in certain states.
Gabapentin is approved by the Food and Drug Administration (FDA) to treat seizure disorders and neuropathic pain.
Some people misuse the prescription medication alongside opioids to boost their effects, though this significantly increasesTrusted Source the risk of unintentional opioid poisoning and death.
This has led several U.S. states to classify gabapentin as a controlled substance, with more potentially looking to do the same.
There have also been calls for the Drug Enforcement Administration (DEA) to classify the medication as a federally controlled substance, though some doctors disagree with such a move.
Read on to find out more about gabapentin’s current classification status across the United States and the various side effects and risks of the medication.
Gabapentin has been a federally noncontrolled substance since its FDA approval in 1993.
It’s typically used for epilepsy and nerve pain, a severe symptom that other prescription medications can often not manage.
But some states do control its use, labeling gabapentin as a Schedule 5 controlled substance.
Although gabapentin isn’t controlled federally, some states have listed it as a controlled substance and therefore regulate its use.
That’s because there have been increasing reports of gabapentin being misused, whether by being combined with opioids or used alone for nonprescribed reasons.
Some neurologists believe that stricter gabapentin regulation may lead to greater opioid use and make it harder for people with neuropathic pain to receive proper care.
The following states classify gabapentin as a controlled substance:
Several other states require gabapentin prescriptions to be monitored, allowing authorities to detect potential misuse:
These lists may be subject to change.
Gabapentin is generally well tolerated and safe for most people to use. But as with any medication, there’s a risk of side effects. Misuse can increase the risk of side effects.
Potential side effects include:
In rare cases, more serious side effects include:
If you experience any of the above symptoms, seek immediate medical attention or contact your local emergency services.
Before taking gabapentin, tell your doctor if you:
When first taking gabapentin, it’s best to be cautious when driving, using machinery, or drinking alcohol. The medication can cause drowsiness, which may affect your ability to do certain things, or have an adverse reaction when mixed with alcohol.
But the biggest risks of gabapentin come when people take the medication with opioids, or if a person already has a substance use disorder. In these cases, there may be an increased risk of dependence or overdose.
Serious breathing troubles can also occurTrusted Source in people with respiratory conditions, like chronic obstructive pulmonary disease (COPD) or asthma, or related risk factors.
Finally, there may be a higher risk of fetal cardiac abnormalities in pregnant people, according to a 2020 study. But the same study did not find evidence of a link between gabapentin use and major fetal abnormalities overall.
Before taking any new medication, it’s a good idea to talk with a healthcare professional.
Let them know if you currently take any opioid medication or medications for anxiety or sleep, or if you have any health conditions, such as breathing disorders, kidney disease, or diabetes.
It’s important to be honest about any drug or alcohol use or misuse. This will help your clinician determine whether gabapentin is safe for you, or if there’s a better alternative.
While there have been calls to make gabapentin a controlled substance across the United States, there are currently only limitations in some states.
Concerns revolve around its use alongside opioids and the potentially dangerous effects of this combination.
Melinda
Reference:
I want to send a special thank you to Dr. Alvin May and Erin Cernuda from Jackson Clara Publishing, LLC for sending me Heal Your Wound to read and review.
Dr. Alvin May is a general surgeon and wound care physician serving the Southern California area for over ten years. He is a graduate of Harvard Medical School and trained in general surgery at the Boston Medical Center. Shortly after starting his career, Dr. May helped launch a national wound care company providing physician-directed wound care services to nursing homes and long-term care facilities.
This book breaks down complex medical concepts into simple, actionable steps. “Heal Your Wound” offers a unique blend of expert advice and real-life stories, showing you exactly how to accelerate your healing process. You’ll uncover the critical factors that might be holding your recovery back, from underlying medical conditions to poor wound care techniques. With practical tips and proven strategies, this book will empower you to take charge of your health.
Available on Amazon

Available on Amazon
Dr. Alvin May was inspired by a personal experience to write on this all to important topic which receives very little attention. One of the first things you will notice is it’s not written in medical talk, the explanations are complete and easy to follow. In addition to his writing, he shares graphics which explains the different types of would and the care needed. If you are in the medical field, a caregiver or caring for yourself this is a must have book for you.
Chronic Wounds: Not your typical wound
The non-healing wound
Wound Healing Basics
A Holistic Approach
Surgical wounds
Dr. May also shares stories of others who have experienced hard to heal wounds.
The journal is invaluable, it provides pages to manage care on a daily and monthly basis, areas to mark medication taken, doctor’s appointments as well as other notes. The journal is a life saver.
Heal Your Wound and the Wound Healing Jornal deserves a permanent place on your bookshelf.
Melinda Sandor
My dinner party would be non-traditional in that each guest is deceased. First it would be multiple parties to talk with everyone I have questions for. The first party would include Jesus, The Virgin Mother, Peter, and Moses. Each shaped my would profoundly and I would love to expaned on certain topics I’m not clear on. I believe Jesus has the ability to see present day but not so much the others. I would love to hear Jesus take on the world today and his new rally cry to Christains. Since the Bible is the foundation of the Christain religion, Jesus might not have anything else to add.
Melinda
There are a number of things you need to know before embarking on a travel adventure. For many people, going on a trip is something they’ve always wanted to do, but it’s not something you can simply just start without any preparation. You need to do a lot of planning and research, and you also need to learn how to control your expectations. Because every location and journey is unique, it’s important to brush up on the essentials before you go; read on to find out more.
If you want to spend less money when traveling, you need to learn how to save money. There are a lot of things that might add up if you approach your adventure like a typical vacation, so it’s vital to spend some time thinking about what’s most important to you. To save money, you may have to give up staying in posh hotels and dining out every night.
Reducing the amount of luggage you bring, learning how to get inexpensive flights, and even traveling in the off-season can all help you save money when you travel. When you’re planning a trip, it’s a good idea to look for ways to save money and tailor your trip accordingly.
What you can and cannot do while you’re gone will be dictated by how you pack, so prepare accordingly. Of course, if you’re just going to stay in one hotel, it doesn’t hurt to bring a few extra things with you since you won’t be dragging them around from place to place. If, on the other hand, you want to travel, you’ll want to learn to pack light since you don’t want to be carrying heavy baggage from place to place and run the risk of losing things on the way.
It’s difficult to pack lightly if you’ve never done it before, but a general guideline is to bring just what you need, bearing in mind that you can purchase some items at your destination if you really need to. Check that you have adequate room for your crucial papers and gadgets that you will need while you are there. You’ll most likely need your phone, a power bank, a camera, and a travel adapter to charge all of your electronics. If you’re planning on camping or hiking, you’ll also need your specialist equipment from ECOGEAR FX.
Depending on where you’re going and the country you’re coming from, you’ll require a different set of paperwork. You may be required to travel with a certain passport and a visa in some cases. If you don’t do your homework in advance, your trip will be a disaster; you might not even get to go in the first place. You should always double-check your understanding of the requirements before proceeding so you aren’t disappointed and don’t lose a lot of money.
Also, it’s a good idea to keep a copy of your papers in a separate location just in case. On top of this, always have all your passport information and additional passport photos with you on any trip. This could save you a lot of trouble if yours goes missing. Having a backup plan in case you lose your passport while traveling might make things a lot less stressful.
This is a collaborative post.
Melinda
Repost
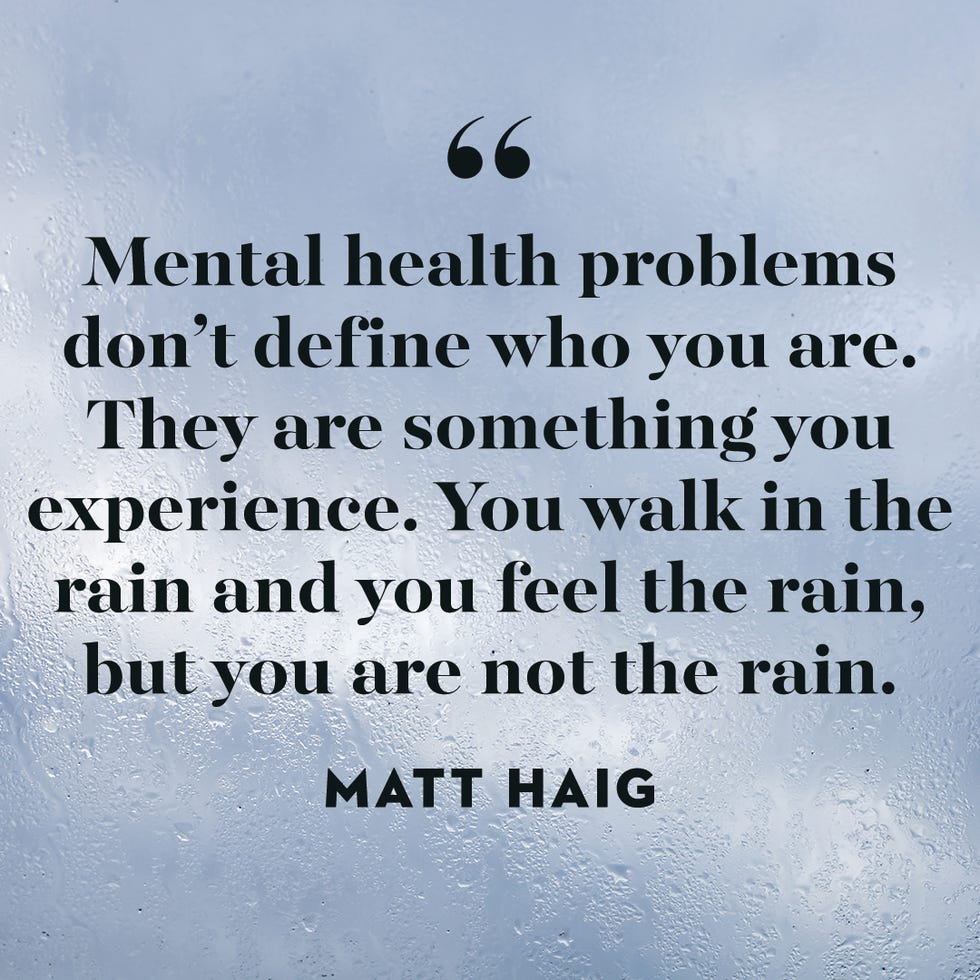
Thank you for joining me for this week’s Friday Quote.
Melinda
It’s the weekend!!!!!!
I’m glad you joined me for another edition of Weekend Music Share this week.
Have a great weekend!
Melinda
Welcome back to Weekend Music Share, the place where everyone can share their favorite music.
Feel free to use the Weekend Music Share banner in your post, and use the hashtag #WeekendMusicShare on social media so other participants can find your post.
I’m so glad you enjoy Fun Facts. I learn something new each week, even if it’s weird. I love hearing your comments!
Enjoy the humor and try not to laugh too hard like I do each week.
Melinda
While over 100 million people in the US alone have allergies, not everyone is born with them, and they can develop as an adult, during childhood, or be present from birth. The only way to know you are truly allergic to something is to be exposed to the potential trigger. And, you can be allergic to thousands of different things. You can have pet allergies, be allergic to bee stings, severe food allergies, and common household materials and chemicals such as hair dyes and cleaning products
In the first instance, you should talk to your doctor if you are concerned you might have an allergy. Your doctor can arrange tests for you to identify if you are allergic to anything and exactly how you are allergic to it. Keep notes of any symptoms and potential triggers you voiced and how you feel. They can talk you through the allergy treatments available and get you started if needed.
Prevention is always better than a cure for allergic reactions, but knowing the signs and symptoms of an allergy attack can help you get the treatment you need fast. Some people only experience mild discomfort when coming into contact with their allergens, for others, it is an instant severe reaction that quickly becomes life-threatening. Know your signs, your triggers, and how best to help yourself. This is especially important if you have yet to be diagnosed, as medical professionals can use this information to analyze your allergy and treat your symptoms quickly.
Common allergy symptoms include;
If you experience these symptoms, you should head to your doctor or pharmacist. In the event of more severe reactions, you should go to the nearest emergency room for immediate treatment.
Some treatment options are available for people with allergies, from using an Epi-pen for more severe reactions, which can be life-saving, to using OTC allergy relief medication. Your doctor can advise you on the right type of medication for you. Be it antihistamines, topical creams for itch relief, desensitization, or immunotherapy to lessen the reaction or avoid the trigger altogether. You can work with them to help you develop a suitable treatment plan based on your lifestyle, specific triggers, and the severity of your reaction. From here, you can adjust your lifestyle to accommodate your allergy and live as healthy as possible.
It is vital that if you are diagnosed with an allergy, you take the proper steps to keep yourself safe. This can be via informing others of your allergy to reduce exposure, carrying around your medication should you need it, or being proactive in asking if your allergens are present in food or environments so you can make a more informed decision. Failure to do this can put you at risk of triggering an allergy, and you will likely suffer the consequences. Always remain vigilant regarding your allergies to ensure you are always prepared.
This is a collaborative post.
Melinda
Repost
I’m glad you joined me on Wordless Wednesday and I hope to see you soon.



We’ve made several homemade pizza’s and the fresh basil in icing on the cake.
Melinda
A new President who focuses on actions that serve the American people and understands international relations.
Melinda
Author Dr. Rita Santos is a clinical psychologist who specialises in cognitive behavioural therapy, anxiety and anxiety disorders.
One of the key symptoms of anxiety is panic attacks. However often, or infrequently, you experience them, it is possible to take steps to change how you react. There are ways that you can loosen their grip, potentially even stopping them from happening altogether.
Using these practical strategies, you can promote understanding, self-awareness, and self-care.
Wellbeck has done it again! They brought us another great self-help book with tools we can implement right away and use for future reference as needed. Dr. Rita Santos gives you real-life examples and tools to use in helping you deal with and overcome Pank Attacks.
Communicating with others
Laying out a self-care plan
Recognizing triggers
and much more.
I recommend this book highly to anyone who has Panic Attacks to understand and communicate with a friend or loved one who does. It’s real-world tips that are easy to implement.
I highly recommend the book and hope you will check it out. It could make a difference for you or someone you love.
Happy Reading
Melinda
I was a child, six months old. You left me in the bathtub while you answered the door. Did you want me to drown?
I was a child, a baby, running a high fever in the middle of winter. You pushed my highchair in front of an open window to cool me down. Did your mother teach you that?
I was a child, a toddler, You dug your nails into my underarms so none would see the bruises. Granny didn’t understand why I cried so hard when you grabbed me by the arm.
I was a child, a teenager. You slapped me for the last time, I fought back. One swing and your husband punches me in the mouth with his fist. Were you glad he came to your rescue?
I was a child, a teenager. You told Child Protective Services I was mentally ill and you were trying to get me admitted to the state hospital. Crazy, who me?
I became an adult, no longer a child, and realized the manipulation and pain you caused and severed all ties. Why do you still send my Birthday and Christmas cards?
I was a child…..
Melinda
Enjoy!
Melinda
Repost
I was on the way to the airport to fly to St. Petersburg, Russia when 9/11 happened, we heard about the disaster on the radio. Back home I called my gramps to ask him if he thought this was the beggining of WW3, he replied it to soon to tell.
The airspace was closed for two weeks before I could make the trip. What was so surprising is people from around the globe were coming up to me to say how sorry they were, some were offering hugs, it was comforting.
The city was more than In could ever ask for, the people, the food, the art, the architecture, the ballet, I could go on. I was told that most women do not travel alone so people would know I was American. The hotel staff took great care of me including calling the restaurants to let them I was coming and to look for me.

View out of my room
I was not alarmed or scared the entire time. Traveling back to St. Petersburg is a desire of mine, the political situation would have to change greatly.
Happy travels.
Melinda

Be safe.
Melinda
I love this song and can’t help but get up and dance, not just phsycaly but also in my heart.
It’s the weekend!!!!!!
I’m glad you joined me for another edition of Weekend Music Share this week.
Have a great weekend!
Melinda
Welcome back to Weekend Music Share, the place where everyone can share their favorite music.
Feel free to use the Weekend Music Share banner in your post, and use the hashtag #WeekendMusicShare on social media so other participants can find your post.
Thank you for joining me for this week’s Friday Quote.

Melinda
It’s hard to define romantic because romance is different to everyone. Romance has to be pure without an agenda or expecting something in return. The action makes you happy as well, meaning that you are happy because they are happy. Romance doesn’t have a price tag or have to be a big deal, a hug or helping to fold clothes works great for me.
Melinda
The 4th of July is one of the most significant holidays in American history as it established that the British were no longer in control of the colonies. The Declaration of Independence paved the way for America to grow as it’s own country.
Independence Day, in the United States, the annual celebration of nationhood held on July 4. It commemorates the passage of the Declaration of Independence by the Continental Congress on July 4, 1776. This document announced the separation of the 13 North American colonies from Great Britain. In 1870 the U.S. Congress made Independence Day an unpaid holiday for federal workers, and in 1938 it became a paid federal holiday. Also called the Fourth of July, the holiday is celebrated across the United States with parades, fireworks shows, picnics, concerts, and other festivities. Independence Day is also notable for its displays of patriotism, as many Americans commemorate the day by flying the American flag and dressing in the flag’s colors of red, white, and blue.

Melinda
Reference:
https://www.britannica.com/topic/Independence-Day-United-States-holiday
It’s exciting to recieve a reminder of the years I’ve been blogging, it’s something I love to do. My writing skills have improved over the years but what is most important is the connections made through my blog. Thank you for your support.

Happy Anniversary with WordPress.com!
You registered on WordPress.com 16 years ago.
Thanks for flying with us. Keep up the good blogging.
My first blog on WP was called Defining Memories which I started in 2005 and closed when I started Looking for the Light. It’s been a wild ride!
Melinda
Gratitude is easy to express, from saying thank you, giving hugs, letting people know you appreciate them or sending a card or text. I’m a card person myself, it feels extra special to me.
Melinda
Your Garden needs gentle care and attention throughout the year. Of course, in the spring and summer, we clean away the winter debris, ready for outdoor parties and barbecues. Or simply just to relax in your little private space.
However, when the winter is coming upon us, leaves from a Fall, as well as the severe weather, can cause damage to your garden. It is very important that you take a couple of steps to get your garden looking gorgeous.
Throughout the autumnal months, there will be many leaves falling, and a lot of rain too. It is very easy for your garden to go from clean and tidy to look a little bit messy, and it eventually will become hard to keep tidy.
Head out and pick up all of the debris; then set it aside because you can use this for a protective layer of mulch for your seedlings.
Take a pair of shears or some secateurs and strip away any loose or dead branches.
If you have furniture in your garden, it is a great idea now to buy some furniture covers; this can protect your furniture when the weather gets more severe. Bring your furniture over the winter months also makes it much easier to clean when springtime comes around.
Now is also the perfect time to cover your barbecue or put it in the shed, ready for use next year.
Depending on what type of pond, you will change how you need to prepare it for the winter months. If you have wildlife in your pond, it is essential that you prepare it correctly for the winter months. Getting a pond maintenance services company out to check over your pond it’s a great idea and can avoid any costly repairs or severe damage over the winter months.
You must start at the bottom and work your way up. Sweep up as much as possible, and also, it is a great time to scrub your patio or your decking. This will mean there is limited damage or weathering over the fall and winter months.
To clean your decking, you simply need to have a firm, stiff brush and apply pressure or use a pressure washer. The pressure washer, of course, being in the fastest way to clean those stains.
After that, move to trimming back trees and bushes, wrapping roots in protective layers, and topping up any birdhouses with food.
If you have plans that are dead or dying, you might have many planters that can be good and used for springtime planting. Remove all of the dead or dying plants and their roots and put them into your compost if you have one.
Most often, the soil can be re-used, so put it somewhere safe ready for your big springtime planting session.
Your garden can be perfect all year round with just a few hours of maintenance here and there.
This is a collaborative post.
Melinda
Repost
I’m glad you joined me on Wordless Wednesday and I hope to see you soon.

Guarding the tomatoe plants.
Melinda
Summer is picking up speed and July brings us new awareness. If you want to see the complete list that included awareness days, click HERE.
Disability Pride Month
Minority Mental Health Awareness Month
National Cleft & Craniofacial Awareness & Prevention Month
Plastic Free July
Sarcoma and Bone Cancer Awareness Month
UV Safety Awareness Month
Wild About Wildlife Month
Take good care.
Melinda
Reference:
https://www.goodgoodgood.co/articles/july-awareness-days-months