The FDA approved the Vagus Nerve Stimulator in 2005 and I was fortunate enough to get approval for it. It’s implanted in my upper left chest, looks like a pacemaker, and the lead wires attach to my Vagus Nerve. I prayed the device would deliver a miracle for my Bipolar Disorder but that was not the case. After several years of adjusting the stimulation, my doctor and I made the decision to turn it off. Almost 20 years later it has become painful and I plan to have it removed this Fall.
The technology has advanced with implants showing better results. I don’t plan to have another implanted but I did find the research on non-invasive VNS devices very interesting. I am researching several brands and will purchase one that vets out. What I find most interesting is the non-invasive devices can help with many other conditions like anxiety, pain, stress, and even migraines. I could use help in many of the areas they tout.
———————
Last updated on July 24th, 2024 at 11:22 am
The human body is a complex and intricate system, with various nerves and pathways working in tandem to maintain optimal health. Among these nerves, the vagus nerve stands out as a key player in regulating numerous bodily functions. Thanks to recent advancements in medical technology, a non-invasive vagus nerve stimulation device has emerged as a breakthrough in the field of medicine. This device has the potential to revolutionize the treatment of various health conditions and enhance overall well-being.
Understanding the Vagus Nerve and Its Functions
The vagus nerve, also known as the tenth cranial nerve, is the longest and most vital nerve in the human body. It extends from the brainstem to various organs, including the heart, lungs, and gastrointestinal tract. The vagus nerve plays a crucial role in regulating essential bodily functions such as heart rate, digestion, and respiratory function.
But what exactly is the vagus nerve, and how does it carry out its functions? Let’s dive deeper into the fascinating world of this remarkable nerve.
The Role of the Vagus Nerve in the Human Body
With its extensive reach and influence, the vagus nerve acts as a communication channel between the brain and various organs. It carries signals that control the parasympathetic nervous system, which is responsible for rest and digestion functions. This means that the vagus nerve helps to slow down heart rate, stimulate digestion, and promote relaxation.
But that’s not all. The vagus nerve also plays a role in modulating inflammation and immune responses. It has been found to have anti-inflammatory effects, helping to regulate the body’s immune system and reduce excessive inflammation. This connection between the vagus nerve and the immune system opens up new possibilities for treating inflammatory diseases.
The Connection Between the Vagus Nerve and Various Health Conditions
Research has shown that abnormalities in vagal nerve activity can contribute to the development and progression of various health conditions. For example, chronic pain has been linked to dysfunctional vagus nerve signaling. By understanding and targeting the vagus nerve, researchers hope to develop new treatments for chronic pain that go beyond traditional pain medications.
Depression and anxiety disorders are also closely tied to vagal nerve activity. Studies have found that stimulating the vagus nerve through techniques like vagus nerve stimulation (VNS) can have a positive impact on mood and reduce symptoms of depression and anxiety. This has led to the development of VNS as a potential treatment option for individuals who do not respond to traditional antidepressant medications.
Migraines, too, have been linked to vagal nerve dysfunction. The vagus nerve is involved in pain modulation, and abnormalities in its function can contribute to the development of migraines. By understanding the role of the vagus nerve in migraines, researchers are exploring new ways to prevent and treat these debilitating headaches.
Furthermore, the vagus nerve’s influence extends to inflammatory diseases. Inflammatory bowel disease, rheumatoid arthritis, and other conditions characterized by excessive inflammation have been associated with vagal nerve dysfunction. This connection has sparked interest in developing therapies that target the vagus nerve to regulate inflammation and potentially provide relief for individuals with these conditions.
As we continue to unravel the mysteries of the vagus nerve, its importance in maintaining overall health and well-being becomes increasingly evident. By understanding its functions and connections to various health conditions, researchers are paving the way for innovative treatment approaches that could improve the lives of millions.
The Evolution of Vagus Nerve Stimulation (VNS) Therapy
Vagus nerve stimulation (VNS) therapy has been used for decades as a treatment option for certain conditions. Traditional VNS involves the implantation of a device that delivers electrical impulses directly to the vagus nerve. While effective in some cases, this invasive approach has limitations and potential complications, leading researchers to explore alternative methods.
The Traditional Approach to VNS
In the past, VNS therapy involved the surgical implantation of a device that connects to the vagus nerve. This device typically delivers mild electrical impulses to modulate the nerve’s activity. However, the invasiveness of this method poses risks such as infection, nerve damage, and complications related to device placement.
Despite these risks, the traditional approach to VNS has shown promising results in the treatment of epilepsy and depression. Studies have demonstrated a reduction in seizure frequency and improved mood in patients who underwent VNS therapy. However, the limitations and challenges associated with invasive VNS have prompted researchers to explore less invasive alternatives.
The Limitations and Challenges of Invasive VNS
Despite its positive outcomes in certain cases, invasive VNS therapy presents several challenges. The necessity for surgical implantation limits its accessibility and increases the potential for complications. Additionally, adjusting the stimulation parameters requires medical intervention, making it less flexible for patients who may benefit from personalized treatment regimens.
Furthermore, the invasiveness of the traditional VNS approach may deter some patients from seeking treatment. The fear of surgery and the associated risks can be a significant barrier, especially for individuals with comorbidities or those who are more risk-averse. As a result, researchers have been actively exploring non-invasive or minimally invasive alternatives to VNS therapy.
One such alternative is transcutaneous VNS, which involves the application of electrical stimulation to the skin overlying the vagus nerve. This non-invasive approach eliminates the need for surgical implantation, reducing the associated risks and complications. Transcutaneous VNS has shown promising results in the treatment of various conditions, including migraine, depression, and chronic pain.
Another emerging technique is minimally invasive VNS, which utilizes a smaller, less invasive device for nerve stimulation. This approach involves the placement of a tiny electrode near the vagus nerve, allowing for targeted stimulation without the need for extensive surgery. Minimally invasive VNS offers a middle ground between traditional invasive VNS and non-invasive alternatives, providing a balance between effectiveness and safety.
As researchers continue to explore and refine VNS therapy, advancements in technology and medical understanding are driving the evolution of this treatment modality. The development of novel devices, improved stimulation parameters, and a better understanding of the underlying mechanisms are all contributing to the expansion of VNS therapy options.
In conclusion, while traditional VNS therapy has been a valuable treatment option for certain conditions, the limitations and potential complications associated with invasive approaches have prompted researchers to explore alternative methods. Non-invasive and minimally invasive techniques are emerging as promising alternatives, offering improved accessibility, reduced risks, and increased flexibility for personalized treatment. As the field of VNS therapy continues to evolve, patients can look forward to more effective and safer options for managing their conditions.
The Advent of Non-Invasive Vagus Nerve Stimulation (nVNS)
Non-invasive vagus nerve stimulation (nVNS) has emerged as an exciting alternative to traditional VNS therapy. This innovation allows for the stimulation of the vagus nerve without the need for surgical procedures or implantation.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and inflammation. Traditionally, vagus nerve stimulation (VNS) has been used as a treatment option for conditions such as epilepsy and depression. However, the invasive nature of VNS therapy has limited its accessibility and acceptance.
nVNS offers a non-invasive solution to harness the therapeutic potential of the vagus nerve. By utilizing mild electrical stimulation, nVNS can activate the vagus nerve and modulate its activity, providing a promising avenue for the treatment of various health conditions.
The Science Behind nVNS
nVNS operates on the principle that mild electrical stimulation can activate the vagus nerve and modulate its activity. By placing electrodes on the skin over specific nerve pathways, nVNS devices deliver targeted electrical impulses, stimulating the vagus nerve indirectly. This non-invasive approach has shown promising results in clinical trials
Research has demonstrated that vagus nerve stimulation can have a profound impact on the body’s autonomic nervous system, which controls involuntary functions. By modulating the vagus nerve’s activity, nVNS can influence heart rate, blood pressure, and even the release of neurotransmitters in the brain.
Furthermore, studies have suggested that nVNS may have anti-inflammatory effects. Inflammation is a key component of many chronic diseases, and by reducing inflammation through vagus nerve stimulation, nVNS could potentially offer a novel therapeutic approach.
The precise mechanisms through which nVNS exerts its therapeutic effects are still being explored. However, the growing body of research indicates that this non-invasive technique holds great promise for the future of medical treatment.
The Design and Function of nVNS Devices
nVNS devices consist of a handheld stimulator with attached electrodes. When applied to specific areas, such as the neck or tragus, these devices deliver precisely calibrated electrical impulses. The stimulation triggers a response in the vagus nerve, which can have therapeutic effects on various health conditions.
One of the advantages of nVNS devices is their portability and ease of use. Patients can conveniently carry the handheld stimulator with them and apply the electrodes whenever needed. This flexibility allows for on-demand stimulation, enabling individuals to tailor their treatment according to their specific needs and symptoms.
Additionally, nVNS devices are designed to be user-friendly, with intuitive controls and adjustable settings. This ensures that patients can easily customize their stimulation parameters, optimizing the therapy’s effectiveness and comfort.
As the field of nVNS continues to advance, researchers and engineers are exploring innovative ways to enhance device design and functionality. Efforts are being made to develop smaller, more discreet devices that can be worn comfortably throughout the day, allowing for continuous vagus nerve stimulation without disrupting daily activities.
Moreover, advancements in technology are enabling the integration of nVNS devices with smartphone applications and wearable devices. This integration offers the potential for real-time monitoring and personalized treatment plans, further optimizing the therapeutic benefits of nVNS.
In conclusion, non-invasive vagus nerve stimulation (nVNS) represents a groundbreaking development in the field of medical treatment. By providing a non-surgical and easily accessible alternative to traditional VNS therapy, nVNS holds immense potential for improving the lives of individuals with various health conditions. With ongoing research and technological advancements, the future of nVNS looks promising, paving the way for a new era of personalized and effective medical interventions.
The Potential Health Benefits of nVNS
nVNS has the potential to offer significant health benefits across a range of conditions, opening up new possibilities for treatment and management.
With its ability to modulate the vagus nerve’s activity, nVNS holds promise in revolutionizing various areas of healthcare. From chronic pain management to mental health treatment, this innovative approach has garnered attention and sparked excitement among researchers and medical professionals alike.
The Impact of nVNS on Chronic Pain Management
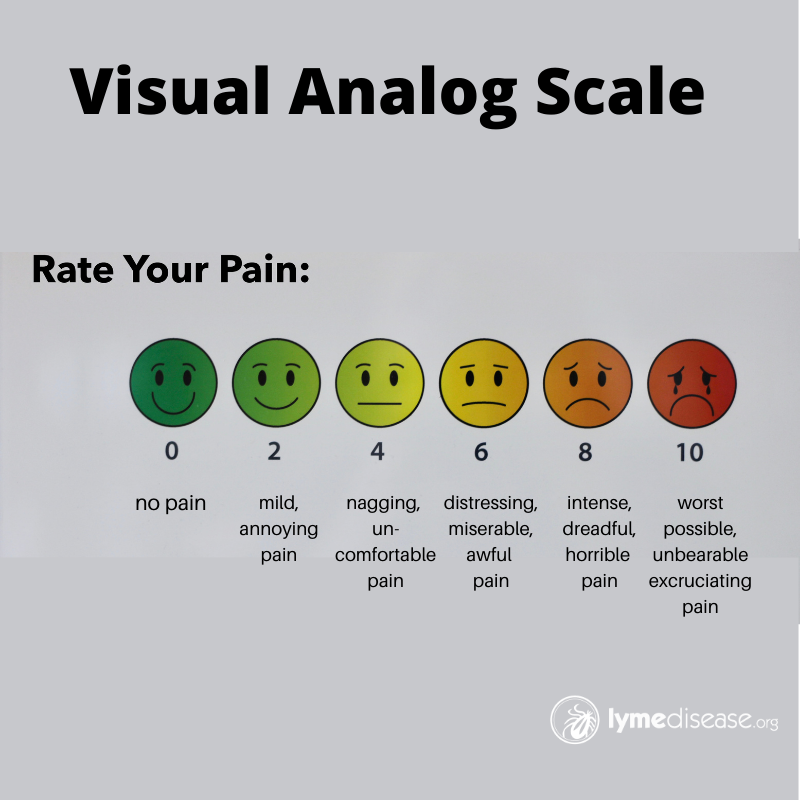
Chronic pain is a widespread and challenging condition that can significantly impact a person’s quality of life. Traditional pain management approaches often involve pharmacological interventions, which may come with unwanted side effects and limited efficacy. However, studies have shown that nVNS can provide effective pain relief by modulating the vagus nerve’s activity.
The vagus nerve, a major component of the parasympathetic nervous system, plays a crucial role in pain perception and inflammation. By targeting this nerve through non-invasive nVNS, it is possible to reduce inflammation and alter pain perception, offering a non-pharmacological approach to pain management. This opens up new avenues for individuals suffering from chronic pain, providing them with a potential alternative or complementary treatment option.
nVNS and Mental Health: A New Frontier
Mental health disorders, including depression and anxiety, affect millions of people worldwide. While various treatment modalities exist, there is a constant need for innovative approaches that can enhance therapeutic outcomes and minimize side effects. nVNS has emerged as a potential game-changer in the field of mental health treatment.
Research has shown that nVNS can modulate the vagus nerve’s activity, influencing neurotransmitter release and mood-regulating pathways. By doing so, it offers a novel and non-invasive approach to mental health treatment. This exciting development has the potential to transform the lives of individuals struggling with mental health disorders, providing them with a new frontier of hope and possibilities.
Furthermore, the non-pharmacological nature of nVNS makes it an attractive option for individuals who may be hesitant or unable to tolerate traditional medication-based treatments. By harnessing the power of the vagus nerve, nVNS opens up a world of potential for personalized and targeted mental health interventions.
As research continues to unfold, the potential health benefits of nVNS become increasingly evident. From chronic pain management to mental health treatment, this innovative approach holds promise in revolutionizing the way we understand and address various health conditions. With its non-invasive nature and ability to modulate the vagus nerve’s activity, nVNS offers a glimpse into a future where personalized and effective treatments are within reach for individuals worldwide.
The Future of nVNS in Medical Technology
As the field of medical technology continues to advance, researchers are exploring additional applications and potential benefits of non-invasive vagus nerve stimulation (nVNS). This innovative therapy has shown promise in various areas of healthcare, and ongoing research is shedding light on its potential to revolutionize personalized medicine.
Ongoing Research and Potential New Applications
Researchers are actively investigating the effects of nVNS on various health conditions and exploring its potential to improve outcomes. One area of focus is epilepsy, a neurological disorder characterized by recurrent seizures. Preliminary studies have shown that nVNS may help reduce the frequency and severity of seizures in some patients, offering a new avenue for managing this challenging condition.
Another area of interest is migraines, debilitating headaches that can significantly impact a person’s quality of life. Early research suggests that nVNS may provide relief for migraine sufferers by modulating the activity of the trigeminal nerve, which is involved in the development of migraines. This non-invasive approach could offer a promising alternative or complement to existing treatments.
Inflammatory diseases, such as rheumatoid arthritis and Crohn’s disease, are also being explored as potential targets for nVNS therapy. These conditions involve an overactive immune response, leading to chronic inflammation and tissue damage. By stimulating the vagus nerve, nVNS may help regulate the immune system and reduce inflammation, offering a novel approach to managing these complex diseases.
Furthermore, researchers are even investigating the potential cognitive enhancement effects of nVNS. By stimulating the vagus nerve, nVNS may modulate brain activity and improve cognitive function. This could have implications for conditions such as Alzheimer’s disease and age-related cognitive decline, where maintaining cognitive abilities is crucial for maintaining independence and quality of life.
The Role of nVNS in Personalized Medicine
One of the most exciting aspects of nVNS is its potential to be tailored to individual patients. With adjustable settings and personalized parameters, nVNS therapy can be optimized to meet each person’s unique needs. This personalized approach has the potential to enhance treatment effectiveness and improve patient outcomes.
For example, the intensity and frequency of nVNS stimulation can be adjusted based on the severity of symptoms and individual response. This flexibility allows healthcare providers to fine-tune the therapy to achieve the best possible results for each patient. Additionally, the ability to remotely monitor and adjust nVNS devices further enhances the personalized nature of this therapy, allowing for real-time optimization and improved patient convenience.
Moreover, the integration of nVNS with other medical technologies holds promise for personalized medicine. By combining nVNS with wearable devices, such as smartwatches or biosensors, healthcare providers can gather real-time data on a patient’s physiological responses and customize nVNS therapy accordingly. This integration could lead to more precise and effective treatment strategies, tailored to the specific needs of each individual.
In conclusion, the emergence of non-invasive vagus nerve stimulation devices represents a breakthrough in medical technology. By harnessing the power of the vagus nerve, these devices offer new possibilities for the treatment and management of various health conditions. The potential benefits of nVNS in chronic pain management, mental health treatment, and other areas are particularly promising. As further research unfolds and technology continues to advance, the future of nVNS holds great potential for revolutionizing personalized medicine and improving the lives of countless individuals.
This is a huge breakthrough for so many people.
Melinda
Reference: