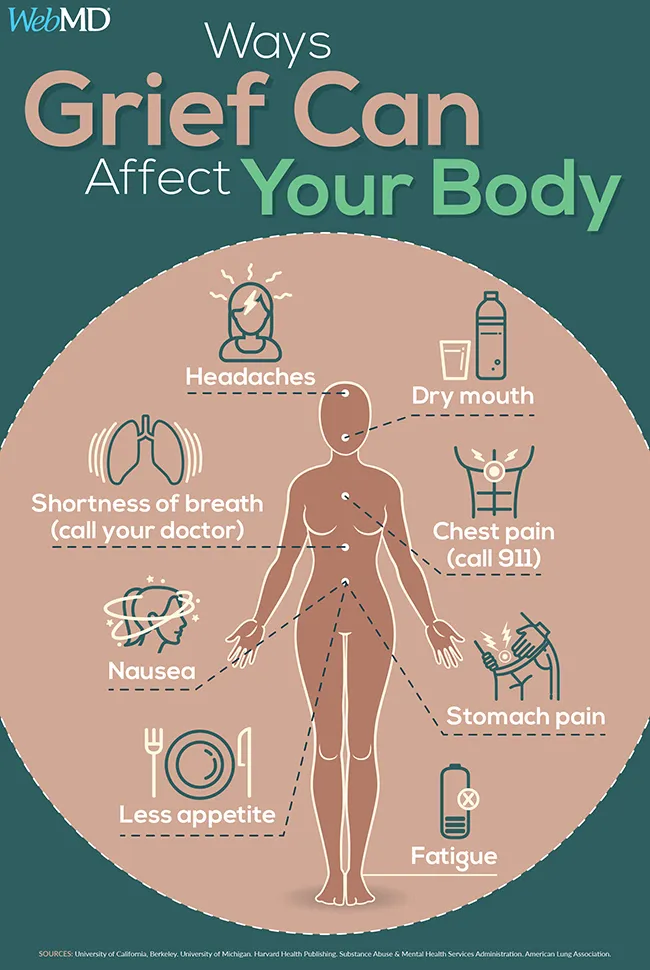
It’s surprising how physical grief can be. Your heart literally aches. A memory comes up that causes your stomach to clench or a chill to run down your spine. Some nights, your mind races, and your heart races along with it, your body so electrified with energy that you can barely sleep. Other nights, you’re so tired that you fall asleep right away. You wake up the next morning still feeling exhausted and spend most of the day in bed.
Amy Davis, a 32-year-old from Bristol, TN, became sick with grief after losing Molly, a close 38-year-old family member, to cancer. “Early grief was intensely physical for me,” Davis says. “After the shock and adrenaline of the first weeks wore off, I went through a couple of months of extreme fatigue, with nausea, headaches, food aversion, mixed-up sleep cycles, dizziness, and sun sensitivity. It was extremely difficult to do anything. … If there’s one thing I want people to know about grief, it’s how awful it can make your body feel.”
What causes these physical symptoms? A range of studies reveal the powerful effects grief can have on the body. Grief increases inflammation, which can worsen health problems you already have and cause new ones. It batters the immune system, leaving you depleted and vulnerable to infection. The heartbreak of grief can increase blood pressure and the risk of blood clots. Intense grief can alter the heart muscle so much that it causes “broken heart syndrome,” a form of heart disease with the same symptoms as a heart attack.
Stress links the emotional and physical aspects of grief. The systems in the body that process physical and emotional stress overlap, and emotional stress can activate the nervous system as easily as physical threats can. When stress becomes chronic, increased adrenaline and blood pressure can contribute to chronic medical conditions.
Research shows that emotional pain activates the same regions of the brain as physical pain. This may be why painkilling drugs ranging from opioids to Tylenolhave been shown to ease emotional pain.
Normal vs. Pathological Grief
Depression is not a normal part of grief, but a complication of it. Depression raises the risk of grief-related health complications and often requires treatment to resolve, so it’s important to know how to recognize its symptoms. Sidney Zisook, MD, a grief researcher and professor of psychiatry at the University of California, San Diego, says people can distinguish normal grief from depression by looking for specific emotional patterns.
“In normal grief, the sad thoughts and feelings typically occur in waves or bursts followed by periods of respite, as opposed to the more persistent low mood and agony of major depressive disorder,” Zisook says.
He says people usually retain “self-esteem, a sense of humor, and the capacity to be consoled or distracted from the pain” in normal grief, while people who are depressed struggle with feelings of guilt and worthlessness and a limited ability “to experience or anticipate any pleasure or joy.”
Complicated grief differs from both depression and normal grief. M. Katherine Shear, MD, a professor of psychiatry at Columbia University’s School of Social Work and director of its Center for Complicated Grief, defines complicated grief as “a form of persistent, pervasive grief” that does not get better naturally. It happens when “some of the natural thoughts, feelings, or behaviors that occur during acute grief gain a foothold and interfere with the ability to accept the reality of the loss.”
Symptoms of complicated grief include persistent efforts to ignore the grief and deny or “rewrite” what happened. Complicated grief increases the risk of physical and mental health problems like depression, anxiety, sleep issues, suicidal thoughts and behaviors, and physical illness.
How Does Avoidance Harm Your Health?
Margaret Stroebe, PhD, a bereavement researcher and professor of clinical psychology at Utrecht University, says that recent research has shed light on many of “the cognitive and emotional processes underlying complications in grieving, particularly rumination.”
Research shows that rumination, or repetitive, negative, self-focused thought, is actually a way to avoid problems. People who ruminate shift attention away from painful truths by focusing on negative material that is less threatening than the truths they want to avoid. This pattern of thinking is strongly associated with depression.
Rumination and other forms of avoidance demand energy and block the natural abilities of the body and mind to integrate new realities and heal. Research by Stroebe, and others shows that avoidance behavior makes depression, complicated grief, and the physical health problems that go with them more likely. Efforts to avoid the reality of loss can cause fatigue, weaken your immune system, increase inflammation, and prolong other ailments.
How Do Role Adjustments Affect Your Health?
When someone close to you dies, your social role changes, too. This can affect your sense of meaning and sense of self.
Before losing Molly, Davis says she found a personal sense of value in “being good at helping other people and taking care of them.” But after Molly died, she felt like she “couldn’t help anyone for a while.” Losing this role “dumped the bucket” of her identity “upside down.” Davis says, “I felt like I had nothing to offer. So I had to learn my value from other angles.”
Caregivers face especially complicated role adjustments. The physical and emotional demands of caregiving can leave them feeling depleted even before a loved one dies, and losing the person they took care of can leave them with a lost sense of purpose.
“Research shows that during intense caregiving periods, caregivers not only experience high levels of stress, they also cannot find the time and energy to look after their own health,” says Kathrin Boerner, PhD, a bereavement researcher and professor of gerontology at the University of Massachusetts in Boston.
“This can result in the emergence of new or the reemergence of existing ‘dormant’ health problems after the death of the care recipient. These health issues may or may not be directly related to the caregiver’s grief experience, but they are likely related to the life situation that was created through the demands of caregiving,” Boerner says.
It can be hard to make life work again after a close family member dies. Losing a partner can mean having to move out of a shared home or having to reach out to other loved ones for help, which can further increase emotional stress and worry. Strobe says the stress of adjusting to changes in life and health during and after a loss can “increase vulnerability and reduce adaptive reserves for coping with bereavement.”
What Can You Do to Cope With Grief?
Emotional and physical self-care are essential ways to ease complications of grief and boost recovery. Exercising, spending time in nature, getting enough sleep, and talking to loved ones can help with physical and mental health.
“Most often, normal grief does not require professional intervention,” says Zisook. “Grief is a natural, instinctive response to loss, adaptation occurs naturally, and healing is the natural outcome,” especially with “time and the support of loved ones and friends.”
For many people going through a hard time, reaching out is impossible. If your friend is in grief, reach out to them.Amy Davis
Grief researchers emphasize that social support, self-acceptance, and good self-care usually help people get through normal grief. (Shear encourages people to “plan small rewarding activities and try to enjoy them as much as possible.”) But the researchers say people need professional help to heal from complicated grief and depression.
Davis says therapy and physical activities like going for walks helped her cope. Social support helped most when friends tried to reach out instead of waiting or asking her to reach out to them.
“The thing about grief and depression and sorrow and being suicidal is that you can’t reach out. For many people going through a hard time, reaching out is impossible. If your friend is in grief, reach out to them. Do the legwork. They’re too exhausted!”
Davis’ advice to most people who are grieving is to “Lean into it. You only get to grieve your loved one once. Don’t spend the whole time trying to distract yourself or push it down. It does go away eventually, and you will miss feeling that connected to that person again. And if you feel like your whole life has fallen apart, that’s fine! It totally has. Now you get to decide how to put yourself back together. Be creative. There’s new life to be lived all around you.
Melinda
Reference:
“WebMD News Special Report Reviewed by Neha Pathak, MD on July 11, 2019