In the future, what will people be nostalgic for from our current time?
Melinda
Reference:
Melinda
Reference:
It seems like there are new myths about Marijuana popping up all the time. The reality is that many of these myths have been disproven long ago. However, they persist in today’s society for one reason or another. Some people believe them because they haven’t done any research on their own. In contrast, others may do so because it benefits them to keep these misconceptions alive. We’ll be giving you the facts about some common myths associated with Marijuana and dispel them once and for all!
You can find this myth in many pro-marijuana campaigns across the world. The truth is that it’s entirely possible to get addicted to Marijuana, just like any other substance out there. Of course, it will not happen overnight, and you shouldn’t be able to do so by smoking one joint either! When people argue about whether or not marijuana addiction exists, they are usually talking about cannabis dependency. This type of dependency occurs when someone smokes on a daily basis for an extended period of time, usually several months. It slowly becomes harder and harder for them to function normally without getting high first.
This doesn’t mean that these individuals have no control over their actions, though; they simply use weed as a crutch because they’re too anxious or uncomfortable without it. The next time you’re around someone who is high, really think about whether or not they look like they need it to function normally.
One of the most common things heard about weed is that it’s safe and harmless to use. This couldn’t be further from the truth! We’ll touch on some key points here, but if you would like more information, then research Marijuana safety tips.
There are many negative health effects associated with smoking marijuana regularly or excessively. For one thing, long-term smokers usually end up getting respiratory problems such as bronchitis because they inhale so much tar and ash into their lungs. If this doesn’t sound healthy to you already, keep in mind that Marijuana contains 50% more carcinogenic hydrocarbons than regular cigarettes do too! There have also been studies showing an increased risk of lung cancer among people who smoke Marijuana regularly.
Getting your Marijuana from the best dispensary possible is an additional factor to consider as there are legislative quality controls they need to follow, ensuring you get a pure and clean product.
This is a controversial point, but it has been proven that Marijuana does not cause people to try out harder drugs. Sure there are cases where this happened due to the influence of others, but overall it would be an unfair label to place on Marijuana.
The problem here lies in the fact that some unscrupulous dealers will sell their customers harder drugs when they come back. It’s not because the Marijuana itself made them do it, but you can’t deny that Marijuana is an easy way to get someone hooked on something else! There are studies showing that people who already have a tendency towards addiction may try harder substances if given access to an alternative like Marijuana in most cases.
The biggest argument for legalizing Marijuana is its medicinal properties. There are many positive uses for Marijuana, both as an analgesic and to help with the symptoms of certain diseases. It makes sense that people who could benefit from this would want access to it without having to wait until the laws change in their state or country!
There has been a wealth of research done in the past several years that have shown Marijuana’s amazing medical value. The US government even holds a patent on Cannabis for its antioxidant and neuroprotectant abilities.
In conclusion, there are many common myths when it comes to marijuana use that simply isn’t true at all! This is especially important nowadays when more and more states are legalizing the drug either recreationally or medically.
This is a collaborative post.
Melinda
Repost
Thank you for joining me for this week’s Friday Quote.

Melinda
The U.S. Geological Survey found that at least 45% of tap water in the U.S. is estimated to have one or more types of PFAS, known as “forever chemicals,” which are linked to serious health issues
Nearly half of the country’s tap water could be contaminated with cancer-causing “forever chemicals,” according to a new study.
The study — released Wednesday by the U.S. Geological Survey — found that at least 45% of tap water in the United States is estimated to have one or more types of per-and poly-fluoroalkyl substances.
The United States Environmental Protection Agency (EPA) states that PFAS, or per-and poly-fluoroalkyl substances, are a group of about 14,000 man-made chemicals that are “very persistent in the environment and in the human body – meaning they don’t break down and they can accumulate over time.”
PFAS, also known as “forever chemicals” by the NIH, can last for years without breaking down and are linked to cancer, fetal complications, liver disease, kidney disease, thyroid disease, fertility problems, autoimmune disorders and other serious health issues.
The USGS said the study is the first to test for PFAS in tap water from both private and public water supplies, testing 716 locations across the country between 2016 and 2021. Of the locations, both rural and urban areas, 447 rely on public water supplies and 269 rely on private wells.
Scientists estimate that there is about a 75% chance of PFAS being found in rural areas and about a 25% chance in urban areas. High exposure areas were reported in the Great Plains, Great Lakes, Eastern Seaboard, and Central/Southern California regions.
“USGS scientists tested water collected directly from people’s kitchen sinks across the nation, providing the most comprehensive study to date on PFAS in tap water from both private wells and public supplies,” said USGS research hydrologist Kelly Smalling, the study’s lead author. “The study estimates that at least one type of PFAS – of those that were monitored – could be present in nearly half of the tap water in the U.S. Furthermore, PFAS concentrations were similar between public supplies and private wells.”
The EPA regulates public water supplies while private water supplies are maintained, tested and treated by homeowners. Anyone interested in testing and treating private wells should contact their local and state officials for guidance as testing is the only way to confirm the presence of PFAS in wells.
“If the average American is worried about the quality of their drinking water, they can use this and other studies to get informed, evaluate their own [personal] risk and reach out to their local health officials about testing or treatment,” Smalling told NPR.
Melinda
Reference:
https://people.com/cancer-causing-forever-chemicals-found-in-nearly-half-of-u-s-tap-water-7557908
Consumers are encouraged to dispose of any contaminated food products immediately
Residents in Sacramento and Davis, Calif., may want to check the eggs in their fridge following a recall from a local distributor.
According to the California Department of Public Health (CDPH), Veg Farms, based in Dixon, Calif., issued a recall on Friday, Dec. 5, due to the potential of Salmonella contamination.
12-count cartons and 30-count flats of eggs with sell-by dates of Dec. 22 and earlier, or Julian dates of 328 and earlier are affected by the recall. Contaminated products with a handler code of 2136 were shipped to both restaurants and farmers’ markets.
:max_bytes(150000):strip_icc():focal(749x0:751x2)/vega-farms-eggs-120925-2-e376d5b1e17c4e46bb87fbf7b3cfef1f.jpg)
A Veg Farms spokesperson confirmed with local news outlet KCRA3 that the company’s processing equipment contaminated the roughly 1,515 dozen eggs, not the farm’s flock of chickens.
Veg Farms stated that it disposed of all of the product from the affected store locations. The company also encourages any consumers who have purchased the eggs to throw them away immediately.
According to the Food & Drug Administration (FDA), symptoms of Salmonella infection can include stomach cramps, diarrhea, fever, headache, nausea and vomiting. While most cases may resolve without medical treatment within a few days, the illness can be more serious (and potentially fatal) for infants, senior adults, people with weakened immune systems and individuals living with sickle cell disease.
:max_bytes(150000):strip_icc():focal(749x0:751x2)/vega-farms-eggs-120925-1-6cc1af1042f246618032d330929f8b23.jpg)
This is only one of the many recalls reported this year due to potential Salmonella infection. Earlier this month, Wegmans, a popular regional grocery store, recalled two types of mixed nuts.
While the company didn’t specify where the Salmonella contamination originated, it’s important to read labels, wash hands and dispose of potentially affected food items to avoid any bodily harm.
Melinda
Reference:
Thank you for joining me on Wordless Wednesday and I look forward to seeing you again soon.

Melinda
Happy New Years Eve!!!!!! We celebrate the end on 2025 and welcome in 2026 with open arms. I haven’t been a party person in over 20 years but sure remember some doozies. If you out and drinking, be sure to have a safe driviner with you, who wants the year to start on very bad note. We celebrate quietly with a table full of finger for and desert and may watch some early New Years Even programs if they are before 9PM. I have a hard core bedtime hour.
Have fun making memories with family, friends reminiscing on the old days and tomorrow you can start thing about what you want to accomplish in 2026. No wish list, wishes down’t come through, make a set of goals and remember to work towards them everyday to manifest them.
See you next year!
Melinda

We have spent 23 years building our finances around living comfortably in retirement and beyond and buying a new house. David retired last April, our house is paid for and we have no debt, just as we planned and saved for.
Yesterday we made an offer on our first house and now David is pulling all the financing together for a mid-February move-in date. I am so in love with the house and have dreamt of living in a one-story without a pool for the longest time.
The seller accepting our offer is just the start. We plan to move into new house, then upgrade our house and sell it. This will be a longer process but I’m screaming inside with excitement.
I’ll give an update if the offer is accepted. We went in with a low offer because it’s been on the market for over a year and no one is living there. The market is down and continuing to go down in our area. Now is the time to buy before the market swings upward.
Melinda :)
Her perspective on life and brutal honesty can help us live our best lives.
Melinda
For years, people living with Lyme disease and other infection-associated chronic illnesses have reported cognitive decline, mood changes, memory problems, and unexplained psychiatric symptoms. Yet these symptoms are routinely dismissed as psychological rather than biological.
At the 2nd Annual Alzheimer’s Pathobiome Initiative (AlzPI) & PCOM Symposium, a new conversation is reshaping that understanding.
In a special live recording of Pathobiome Perspectives, author and Galaxy Diagnostics CEO Nicole Bell shares how her family’s search for answers revealed the role of infection in her late husband Russ’s devastating neurological decline.
In her presentation, “When the brain pathobiome becomes personal,” Bell describes laboratory findings from Russ’s donated brain, including:
These data, now being prepared for publication, reinforce a growing scientific model: polymicrobial infection and toxic exposures may converge to drive neuroinflammation and Alzheimer’s-like symptoms.
Bell also outlines why so many patients fall through the cracks:
She highlights hallmark Bartonella clues often mistaken for psychological disorders — irritability, anxiety, OCD, tics, vision changes, and stretch-mark-like striæ — noting that exposure risk extends beyond ticks to fleas and household cats. Bell advocates for precision diagnostics that assess pathogen load, immune dysfunction, and toxic exposures together, rather than in isolation.
Bell’s story underscores a pivotal shift: what looks psychiatric or “idiopathic” may be a complex, biologically driven pathobiome process — and recognizing it early could change outcomes.
Tune in to this episode of Pathobiome Perspectives, presented in collaboration with Tick Boot Camp and LymeDisease.org, to learn how cutting-edge research could transform our understanding of chronic illness and cognition–and offer hope to millions navigating life through the haze.
Pathobiome Perspectives was developed in collaboration with the Pathobiome Research Center at PCOM, led by Founding Director Nikki Schultek, and Director Dr. Brian Balin and the Center for Chronic Disorders of Aging (CCDA).
New episodes of Pathobiome Perspectives will roll out every Tuesday night at 7:30 p.m. Central.
Ali Moresco is a tick-borne disease survivor, advocate, speaker and founder of Moresco PR, a healthcare communications firm. She also serves as Executive Board Chair of Project Lyme. You can connect with Ali on Instagram at @AliTMoresco or on YouTube.
Melinda
Reference:
“Forever chemicals” are synthetic compounds found in products like non-stick pans, waterproof clothing, dental floss and more items
Researchers have found a new link between exposure to “forever chemicals” — synthetic compounds found in non-stick pans, waterproof clothing, dental floss and more items — and one lifelong health condition.
A new study, published in the scientific journal Environment International, found that people exposed to two major environmental toxins — known as perfluorooctane sulfonic acid (PFOS) and polychlorinated biphenyls (PCBs) — are more likely to be diagnosed with multiple sclerosis, or MS.
“We saw that several individual substances, such as PFOS and two hydroxylated PCBs [substances that arise when PCBs are broken down in the body], were linked to increased odds for MS,” Kim Kultima, who led the Sweden-based study, said in a press release.
“People with the highest concentrations of PFOS and PCBs had approximately twice as high odds of being diagnosed with MS, compared with those with the lowest concentrations,” she added.
According to the Mayo Clinic, multiple sclerosis is a chronic autoimmune disease that causes a breakdown of the protective covering of nerves, causing numbness, weakness, trouble walking, vision changes and other symptoms.
MS causes an interruption in communication between the brain and the rest of the body, and can eventually lead to permanent damage of the nerve fibers.
In this study, researchers analyzed blood samples from 900 people who had been recently diagnosed with MS, and compared them to samples from people who do not have MS.
Kultima and her team then measured the toxin levels in each group’s blood samples, using statistical models see how chemical exposure corresponded with the odds of developing MS. According to the study, people are often exposed to a mixture chemicals at the same time, so researchers also investigated how exposure to more than one toxin affected them.
“We could then see that an increase in total exposure was linked to higher odds of MS, even after adjusting for previously known lifestyle and genetic risk factors,” said Aina Vaivade, the first author of the study.
The final phase of the study also explored the relationship between genetics, chemical exposure and the odds of being diagnosed with MS.
Researchers found that people who carry a certain gene variant have a reduced risk of MS. People who carry the gene and participated in the study saw “unexpected increased odds” of being diagnosed with MS when they had higher PFOS exposure.
“This indicates that there is a complex interaction between inheritance and environmental exposure linked to the odds of MS,” Kultima added.
Melinda
Reference:
The product should be thrown away and not consumed, per the U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS)
A food production company in Georgia has issued a nationwide recall for more than 60,000 lbs. of chicken that was shipped to restaurants across the United States.
The company, called Suzanna’s Kitchen, issued the recall on “approximately 62,550 pounds” of its eight-piece cut, fully-cooked, bone-in breaded chicken product “due to misbranding and an undeclared allergen,” per the U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS).
The product contains soy, which is a known allergen, but it is not listed on the label, per FSIS.
The chicken was produced on Oct. 16, 2025, and has case code “P-1380 126237 B30851 23:11 K04” printed on the side of the packaging. It is shipped in 18 lb. cases containing four units.
FSIS is currently “concerned that some product may be in restaurant refrigerators or freezers,” and restaurants are urged to throw the chicken away should they have it, per the recall.
FSIS first became aware of the contamination when they were alerted to the issue by Suzanna’s Kitchen, which realized some of the chicken had been mislabeled, per the recall statement.
Melinda
Reference:
https://people.com/more-than-60000-lbs-chicken-recalled-nationwide-what-you-need-to-know-11868792
Keep the feedback coming, I sure enjoy your comments each week.
Enjoy!
Melinda
What happens to those dogs that are just too much dog for people to handle? “You know them — you go to your friend’s barbecue, their dog is so happy to see you that she pees on your feet, and she drops a slobbery ball in your lap,” says Megan Parker (TEDxJacksonHole talk: Dogs for Conservation), a wildlife biologist and dog expert based in Bozeman, Montana. “You throw it to get as much distance between you and the dog as possible, but she keeps coming back with the ball. By the 950th throw, you’re thinking, Why don’t they get rid of this dog?” All too often, their owners reach the same conclusion and leave their pet at a shelter.
Thanks to Parker and the team at Working Dogs for Conservation (WD4C), some of these dogs have found a new leash lease on life. They’re using their olfactory abilities and unstoppable drive in a wide variety of earth-friendly ways, working with human handlers to sniff out illegal poachers and smugglers, track endangered species, and spot destructive invasive plants and animals.

Parker first considered using dogs in conservation when she worked on the reintroduction of wolves to Yellowstone Park and was asked how researchers could track wolves through their scat, or droppings. “I started thinking how best to detect their scat off a large landscape, and the idea came up for dogs,” she says. In 2o00, she cofounded WD4C to train and use canines in conservation work. Most of their dogs are adopted from shelters or from organizations or work settings where they didn’t quite fit in.
While it’s fair to say almost all dogs love toys, wildlife-detection dogs areobsessed with them. “They’ll do anything to chase a ball or a tug toy,” says Parker. If their preferred plaything is thrown far into the brush or buried in a massive pile of leaves, no worries — they won’t stop looking until they find it. No food, obstacle or distractions can deter them, and WD4C staff have turned this single-minded focus into a powerful incentive. Their canine friends are rewarded with their favorite toy every time they locate a desired wildlife-related scent, anything from elephant ivory and poachers’ guns in Zambia and trafficked snow leopards in Tajikistan to predatory Rosy wolf snails in Hawaii and invasive Argentine ants on California’s Santa Cruz Islands. The dogs are careful not to disturb or touch any specimens they pinpoint; it’s all about the toy.
Lily, a yellow Lab, is one of the group’s many sad-start-happy-ending stories. When the then-three-year-old came to the attention of WD4C trainers, she’d already bounced her way in and out of five different homes. She couldn’t sit still and she never, ever wanted to stop playing. Oh, and she was a bit of a whiner. Since joining WD4C in 2011, she has been trained to recognize a dozen different conservation-related scents and been deployed to track grizzly bears and sniff out the eggs, beetles and larvae of emerald ash borers, an insect that has killed millions of trees in the US and Canada.

The three-dozen-strong WD4C pack also includes purebred working dogs who weren’t right for their intended occupations. Orbee, a border collie, had the enthusiasm and live-wire energy required of ranch dogs, but there was one problem: he had zero interest in herding sheep. He also barked a lot. Since joining WD4C in 2009, Orbee has had a globe-trotting career — he has spotted invasive quagga and zebra mussels on boats in Alberta and Montana, monitored the habitats of the endangered San Joaquin kit fox in California, and assisted scientists in northern Africa in counting up Cross River gorillas, the world’s rarest gorilla.
Jax is a Belgian malinois, a sturdy breed frequently used by the police and military. He was in training to serve with the US Army’s special unit, the Green Berets, until his handlers realized Jax doesn’t like to bite people — just toys. And, boy, does he loves toys; he’s even tried to climb trees to reach prized objects. Since 2017, Jax’s athleticism and high spirits have been used by the WD4C to perform tasks such as mapping the movements of bobcats in the western US.

“Different dogs have different strong suits,” says Parker. She and the WD4C team try to place their charges in environments that match their skillset, likes and dislikes. Unlike many dogs, Tule (above), a Belgian malinois who flunked out of a job with US Customs and Border Patrol, has absolutely no desire to chase small animals such as cats, squirrels and rabbits. This made her the perfect fit to help researchers monitor black-footed ferrets, which live in the same territory as a large, scampering prairie-dog population. The ferrets, once thought extinct in the US, were reintroduced in Wyoming in recent years. Tule alerts her handlers to the scent of live ferrets or their scat, information that allows state wildlife officials to map their distribution and see if the population is recovering. Without Tule and her pack, researchers would be forced to study the elusive creatures with cameras or live traps, undependable methods at best.
The dogs’ efforts have resulted in positive, substantial changes. The organization teamed up with the nonprofit Wildlife Conservation Society so their dogs could track the scat of four keystone carnivores (grizzly bears, black bears, mountain lions and wolves) through the Centennial Mountains in Idaho and Montana. Five years of doggie data showed that all four species depended on the mountains to move between the Greater Yellowstone ecosystem and central Idaho wilderness areas. Thanks to this information, activists were able to stop construction of a housing development that would have interrupted their migratory pathway.

Some dogs are searching for animals and plants that are most wanted for the opposite reason: they’re invasive species proliferating where they don’t belong and driving out native flora and fauna. There’s the previously mentioned zebra and quagga mussels, which spread by clinging to boats and watercraft, and which clog water and sewage pipes, foul up power plants, and destroy good algae. Tobias (above) is a specialist in finding them. In one test, WD4C dogs identified 100 percent of the boats with mussels aboard (human screeners spotted 75 percent). The dogs did the job more quickly, and they could also detect the mussels’ microscopic larvae.
Former shelter dog Seamus (shown at the top of the post), a border collie, is an expert in searching out dyer’s woad on Mount Sentinel in Montana.Humans have tried to eradicate the invasive weed by spotting its flowers and pulling out plants by hand, but these attempts barely made a dent. By the time it’s found, it’s often already seeded (and a single plant can produce up to 10,000 seeds). Seamus’s keen nose, along with those of three canine colleagues, learned to sniff out woad before it flowered, a time when it’s extremely hard for human eyes to see. They also found root remnants left in the ground. At a recent checkup, just 19 of the invasive plants were found on the mountain. “It will be a complete extermination,” says Parker. “It’s just going to take a long time because we don’t know how long their seeds last in the soil.”
The dogs’ hunting grounds even extend into the water. Although prized in their native habitat, brook trout are an invasive species elsewhere; in some places in the Western US, they are pushing out the native cutthroat trout. WD4C was brought to Montana by the US Fish and Wildlife Service, the US Geological Survey and the Turner Endangered Species Fund to see whether their animals could learn to sniff out live fish in moving water. Reports Parker, “This project confirmed what we long suspected: that dogs can detect and discriminate scents in water.”

Pepin (above), who worked on the brook trout project, is part of an ambitious charge to train the dogs to detect infectious diseases in animals.“He’s done the first of a lot of things for us, because he’s so game,” says Parker. Some wildlife carry brucellosis, a bacterial disease that is particularly harmful to cattle. It’s difficult to tell when animals are first infected because they typically don’t display symptoms, so in areas where the disease is prevalent, ranchers tend to keep livestock and wildlife as far away from each other as possible — severely limiting the territory and movement of both kinds of animals. The hope is that dogs could provide a fast, reliable way to identify infected herds. So far, Pepin has shown he can discriminate infected elk scat with higher and lower concentrations of the bacteria, and W4DC is eager to explore this use of dog power. “We have proof of concept,” says Parker. “I’d like to move that work forward.”
There are so many other unexplored capacities and environments where dogs could help, Parker believes. To that end, WD4C started a program in 2015 called Rescues 2the Rescue, which aims to help shelters around the world identify would-be detection dogs and place them with wildlife and conservation organizations. What kind of dogs are they looking for? Ones that are, uh, crazy.
To clarify that adjective, we’ll close by telling you about Wicket, a black Lab mix who retired from WD4C in 2017 at the top of her game, having detected 32 different wildlife scents in 18 states and seven countries. Wicket languished in a Montana shelter for six months, barking up a storm and scaring away potential owners, until WD4C cofounder Aimee Hurt found her there in 2005. When she went to adopt her, the shelter director said, “You don’t want that dog — that dog’s crazy!” To which Hurt replied, “I think she might be the right kind of crazy.”
Thank you for joining me for this week’s Friday Quote.

Melinda
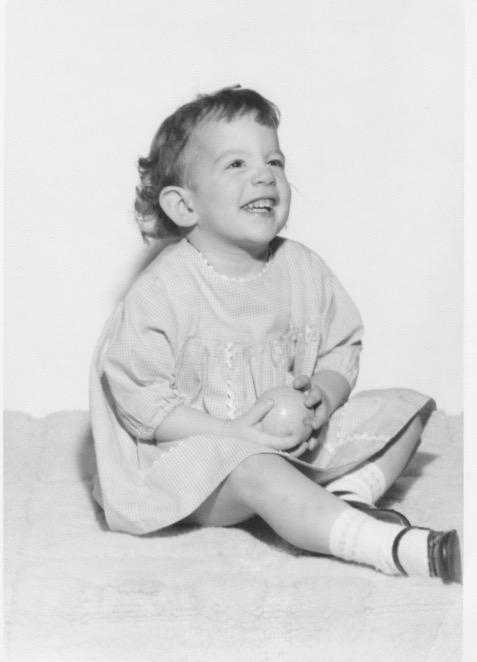
Growing up I couldn’t wait to arrive at my Grandparent’s house for Christmas. My Granny would go over the top with food and sweets. We opened our presents on Christmas Day. They usually bought lots of clothes. I still have all of their ornaments, they are frail, and I don’t use them but I have them to look at and bring back old memories.
Today we celebrate the birth of Jesus, the son of God. Please take a minute to think of the reason for the season.
Around 12 years old
Have a blessed Christmas, I hope you have family and friends to celebrate with and enjoy a good meal by starting with thanks to God for sending his only son who died for our sins..Melinda
Melinda
Growing up our family didn’t have any traditions, we just waiting for Santa. If we were celebrating Christams with my Grandparents and the holiday fell during the week, Gramps had to work and we had to wait all day until he came home from work, it felt like forever.
At 27, I decided to make Christmas Eve a celebration as well. Presents were opened in the early evening followed by a table full of hard meats, cheeses, crackers, olives and desert. For me it was an evening to make special memories more centered on relationships, walks down memory lane, expressing joy and love.
On Christmaas we have a full meal focused on the birth of Jesus and how blessed we are.
What are your Christmas Eve traditions? I love to hear all the ways people celebrate.

Melinda
Thanks for joining me on Wordless Wednesday, I appreciate you.


Melinda
Before we move into the new year, I want to thank you for your kindness. I stopped judging my blog’s success by the numbers, engagement is what’s most important to me. You’ve contributed greatly to the success of Looking for the Light and I thought a glace at the numbers would reflect your contribution.
In 2025 to date there have been 35,034 views
686 Post
16.2K Visitors
21.9K Likes
4K Comments
137 countries stopped by to date
39 Referreral Sites

You have brought me enlightenment, support, motivation and inspiration with each of your posts.
Numbers are a form of measurement however that is not how I judge the health of my blog. Engagement in the form of likes and comments are how I judge if my blog is successful.
Each conversation makes me smile, when a new country visits it intrigues me, having long tern followers are special and all of these help me grow.
Here’s to 2026!
Melinda
Let’s shine a black light on it, so you can know where the smell is coming from. You already know that basically everything in the media is there to sell you thinness — the shellacked abs in ads for exercise equipment, the “one weird trick to lose belly fat” clickbait when all you wanted was a weather forecast, and the “flawless” thin women who fill most TV shows. The Bikini Industrial Complex, or BIC, has successfully created a culture of immense pressure to conform to an ideal that is literally unobtainable by almost everyone and yet is framed not just as the most beautiful, but the healthiest and most virtuous.
But it’s not just magazine covers, ads and other fictions that get it wrong. The body mass index (BMI) chart and its labels — underweight, overweight, obese, etc. — were created by a panel of nine individuals, seven of whom were “employed by weight-loss clinics and thus have an economic interest in encouraging use of their facilities,” as researchers Paul Ernsberger and Richard J Koletsky put it.
You’ve been lied to about the relationship between weight and health so that you’ll perpetually try to change your weight.
But listen: It can be healthier to be 70 or more pounds over your medically defined “healthy weight” than just five pounds under it. A 2016 meta-analysis in The Lancet medical journal examined 189 studies, encompassing nearly four million people who never smoked and had no diagnosed medical issues. It found that people labeled “obese” by the CDC have lower health risk than those the CDC categorized as “underweight.” The study also found that being “overweight” according to the CDC is lower risk than being at the low end of the “healthy” range as defined by the US federal government and the World Health Organization.
Another meta-analysis even found that people in the BMI category labeled “overweight” may live longer than people in any other category, and the highest predictable mortality rate might be among those labeled “underweight.” Taking it further, newer research is suggesting that doctors warn their middle-aged and older patients against losing weight, because the increasingly well-established dangers of fluctuations in weight outweigh any risk associated with a high but stable weight.
Our culture has primed us to judge fat people as lazy and selfish. And it goes deep. Amelia conducts a children’s choir, and she has to teach her kids to breathe. At ten, eight, even six years old, they already believe that their bellies are supposed to be flat and hard, so they hold their stomachs in. You can’t breathe deeply, all the way, without relaxing your abdomen, and you can’t sing if you can’t breathe. So Amelia has to teach children to breathe.
Please: Relax your belly. It’s supposed to be round. The BIC has been gaslighting you.
We’re not saying the people or companies that constitute the BIC are out to get you. Frankly, we don’t think they’re smart enough to have created this system on purpose. But they recognize there’s money to be made by establishing and enforcing impossible standards.
We all encounter the BIC every day. So how can we make it through the fray?
One strategy: Play the “new hotness” game.
When we reconstruct our own standard of beauty with a definition that comes from our own hearts and includes our bodies as they are right now, we can turn toward our bodies with kindness and compassion. Well, easier said than done.
Amelia is vain about pictures of her conducting, in which she inevitably has her mouth wide open and her hair is a sweaty wreck. Emily watches herself on TV and worries that her chin is too pointy because one time, somebody said it was. (We are identical twins.)
Neither of us has ever had the skinny proportions of a model, and we watched our mom — who was model-thin before she gestated two seven-pound babies at the same time — look at her reflection in mirrors and cry at what she saw there. What she saw there is very much like what we see in our own reflections now.
Which is why we play the “New Hotness” game, a way to let go of body self-criticism and shift to self-kindness. One day, Amelia was at a fancy boutique, trying on gowns for a performance. Attire for women conductors is hard to find: solid black with long sleeves, formal yet not frumpy is an unlikely combination. Finding all of this in her size is even more difficult.
She tried on a dress that looked so amazingly good she texted Emily a dress selfie, with a caption paraphrasing Will Smith in Men in Black II: i am the new hotness.
And now “new hotness” is our texting shorthand for looking fabulous without reference to the socially constructed ideal. We recommend it. It’s fun.
Maybe you don’t look like you used to, or like you used to imagine you should, but how you look today is the new hotness. Even better than the old hotness.
Saggy belly skin from that baby you birthed? New hotness.
Gained 20 pounds while finishing school? New hotness.
Skin gets new wrinkles because you lived another year? New hotness.
Hair longer or shorter, or a different color or style? New hotness.
Mastectomy following breast cancer? New hotness.
Amputation following combat injury? New hotness.
The point is, you define and redefine your body’s worth, on your own terms. It’s not necessary to turn toward your body with love and affection — love and affection are frosting on the cake of body acceptance, and if they work for you, go for it. But all your body requires of you is that you turn toward it with kindness and compassion, again and again, without judging all your contradictory emotions, beliefs and longings.
No doubt after you finish reading this, you will go out into the world and notice the diversity of bodies around you. And you will still have reflexive thoughts about the people who don’t conform to the aspirational ideal, envious thoughts about the people who do, or self-critical thoughts about the ways the world tells you that you fall short. And then you might even have emotional reactions to your emotional reactions: “Darn it, I shouldn’t think that!”
Change happens gradually. Your brain has been soaking in the BIC for decades; any time you step outside your door, you’re back in it; any time you turn on a TV, you’re back in it; and any time you put clothes on, you’re back in it. Just notice it, as you’d notice a fleck of dust floating through the air. Smile kindly at the mess. And know what’s true: Everyone is the new hotness. You are the new hotness. So is she. So are they. So are we.
Excerpted from Burnout: The Secret to Unlocking the Stress Cycle by Emily and Amelia Nagoski. Copyright © 2019 by Emily and Amelia Nagoski. Used by permission of Ballantine, an imprint of Random House Publishing Group, a division of Penguin Random House LLC. All rights reserved. No part of this excerpt may be reproduced or reprinted without permission in writing from the publisher.
Melinda
Each month there is a long list of awareness months, days and weeks, To keep the post short I only write about the awareness months. To read to complete list CLICK HERE or the link at bottom of post.
Many of the awareness months hit close to home for me, not only through experience but as missions I’m dedicated to by advocating and sharing information with you.
Melinda
Reference:
Melinda
The post talks about how positive thinking and affermations help with Bipolar Disorder, the truth is everyone can benefilt from the post. What we think and say is what our brain believes.
Words — whether spoken or thought — carry incredible weight. They are capable of healing or harming. The unkind phrases people tell themselves so often can easily turn into beliefs, shaping an unfair and cruel view of who they are.
If words hold so much sway, why, then, can’t they be used for good?
What if your words and what you tell yourself hold the key to a better life? Imagine if, instead of riding along with the usual negative stream of consciousness, you said aloud: “I am worthy.” “I have the strength to overcome any challenge.” “I have come this far — I am capable.”
Appropriately termed “affirmations” or “self-talk,” these are positive statements that can help you confront and overcome self-sabotaging and negative thoughts and beliefs. When you repeat them often and believe in them, you can start making positive changes and rewriting your story.
Most people spend much of their waking time talking to themselves, although they might not always be aware of it. And that internal chatter is much more influential than many realize. Mood is created by the balance of chemicals in the brain — neurotransmitters like dopamine, serotonin, endorphins, and so on.
Yet even your thoughts or self-talk can alter your brain’s chemical reactions, shaping emotions and behaviors. What you say to yourself has real-world consequences.
“What you tell yourself is how you are programming your internal navigation system,” says Jill Sylvester, LMHC, MEd, who has a private practice in Hanover, Massachusetts, and is the author of Trust Your Intuition: 100 Ways to Transform Anxiety and Depression for Stronger Mental Health.
In this way, a person’s inner speech functions much like an internal compass or brain-based GPS. The tone of this self-talk influences our feelings, judgments, self-esteem, and actions — guiding them to move forward, change course, or settle into the status quo.

Sylvester’s metaphor is fitting and raises an important question: If someone isn’t paying attention to their self-talk, who is at the wheel? And where, exactly, are they going?
Repeated often enough, this silent self-address ultimately establishes a person’s default or foundational beliefs about themselves, those around them, and the world in general. So, in a sense, engaging in mindless self-talk is a lot like living on autopilot.
Even so, anyone can take back the controls. That voice in your head, after all, is your own.
The notion of thinking good thoughts is at the center of much psychotherapy, in fact. Reframing your negative thoughts is a powerful way to heal from past trauma. Furthermore, thinking positively to make yourself feel better is not self-deception, says Gregory L. Jantz, PhD, founder of the Center: A Place of Hope, one of the leading facilities for the treatment of depression.
In his book Moving Beyond Depression, Dr. Jantz writes that positive self-talk is “not mentally looking at circumstances with eyes that see only what you want to see. Rather, positive self-talk is about recognizing the truth in situations and in yourself…. [It] allows you to discover the obscured optimism, hope, and joy in any given situation.”
Lorenzo L. of New York City knows this firsthand. In his youth, Lorenzo struggled with “massive mood swings” that much later would be recognized as symptoms of bipolar disorder. Showing wisdom beyond his years, Lorenzo lifted himself out of depressive states by slowing his breathing and using positive affirmations.
With regular meditation, Lorenzo has learned to quickly identify his state of mind. Once he is fully aware of his current mood, he directs his self-talk accordingly: “When I’m coming down from mania or hypomania,” he says, his mantra is, “‘Don’t doubt yourself today. It’s okay that you don’t feel as joyful or productive today.’”
“When I’m cycling up to mania or hypomania,” he continues, “I say, ‘Try not to get too carried away. Use all of this extra energy for productive and healthy activities.’”
And when he is feeling balanced, he uses positive, encouraging inner speech to continue his sense of stability: “I can sustain this mood for more than this moment or day.”
“Self-affirmations,” Sylvester explains, “are positive statements that put a person in the driver’s seat of their life and create a path from which to grow.”
And grown he has. Working full-time and studying to become a certified public accountant, the 37-year-old Lorenzo credits his healthy mindset to meditation and cognitive behavioral therapy (CBT). With the help of his psychologist, he has solidified his initial forays into mindfulness and self-affirmation into a practical, tried-and-true strategy that improves his mood and alleviates his symptoms.
When the terrain is rocky and you’re struggling to stick to your wellness plan, positive self-talk can help you persevere by encouraging you to become proactive instead of reactive. In fact, you can harness your inner monologue to promote what psychologists call “self-regulation” — your ability to exert conscious control over emotional and physical responses to external situations.
You can strengthen your self-regulation by consciously distancing your thoughts from your experiences. One way to do this is to switch your self-talk from first person (“I,” “me,” “my”) to third person — using your own name instead.
An older randomized controlled trial found that doing so during times of stress fosters a sense of perspective, with net benefits including decreased anxiety, improved performance, and faster, more complete emotional recovery.
So, if you’re feeling anxious about an upcoming event or want to gain a bit of emotional separation from an experience to change your response, consider replacing “I” with your name when speaking or thinking your affirmations.
In times of overwhelm, it can be helpful to remind yourself who you are and what defines you as an individual. From there, you can make better decisions.
When Cheryl W. M. faces negative thoughts, she tells herself, “I don’t sweat the small stuff.”
By linking her desired mindset to her self-image in this way, she makes it easier to follow through with her goal of not letting minor inconveniences or difficulties become roadblocks.
Cheryl explains that her affirmation “helps to keep me centered and positive.”
Science supports Cheryl’s experience. In one study, participants with high levels of chronic stress showed reduced problem-solving ability. However, those who engaged in a brief self-affirmation activity performed significantly better on challenging tasks than those who didn’t.
This suggests that self-affirmations can protect against the negative effects of stress, such as impaired creativity and problem-solving.
Confirming the importance of linking affirmations to your identity, Sylvester says that empowering affirmations work best when they begin with “I am,” such as “I am true to myself,” “I am capable,” or “I am smart.” Set in the present tense, they “affirm that things are happening in the present, versus in the future.”
This is when first-person self-talk can prove beneficial, eliminating the emotional distance between your identity and what you want to affirm.
Kim S., understands the power of using self-talk in this way. Every time she looks in the bathroom mirror, she tells herself that she loves herself; then she says, “I am surrounded by love. I am strong today. I can make it right now, just for right now.”
In addition to using “I am” statements that focus on the current moment, Kim, who’s in her early sixties, also imagines being surrounded by white, healing light and beautiful hearts. “And if I have to,” she continues, “I repeat this five times per day.”
When you’re dealing with bipolar depression, it might feel inauthentic or untrue to say to yourself, “I am happy” or “I am capable.” Depression feels heavy and can often rob you of the belief that you can get out of bed, continue with your routines, and return to happiness. At these times, it’s essential to remember that your brain is mistaken.
Clinical psychologist and author of Overcoming the Destructive Inner Voice, Robert W. Firestone, PhD, identifies the “critical inner voice” — the stream of negative, self-defeating, and highly critical self-talk — as the “enemy within.” He writes that this enemy can be overcome only by recognizing it and actively working against it.
By distancing yourself from the “enemy within” and aligning with your true identity through positive, emotionally charged affirmations, you can move toward a more balanced and uplifting state of mind.
That sense of control can feel especially empowering when your mood seems to dictate your days.
Because internal self-talk influences both beliefs and behavior, cultivating awareness of that inner voice enables more intentional, affirming thought patterns.
Lorenzo says, “I know it’s difficult. If you’re struggling, there are ways to adapt your lifestyle and cope with difficult emotions. Such as, for me, affirmations and positive self-talk.”
“It’s a journey,” he says, “for sure.”
There are many ways to increase your sense of personal power and inject some positivity and affirmations into your daily routine. Here are a few to get you started.
Our mental health stays balanced from many forms of help and we need to look at all angles.
Melinda
Reference:
Around 9,400 of CreateOn’s Crayola-branded pip-cubes have been recalled
This story has been updated to reflect that the manufacturer of the recalled toys is CreateOn, not Crayola. The recalled pip-cubes were Crayola-branded, a representative for Crayola confirmed to PEOPLE.
A recall has been issued for toys that could potentially kill or injure children.
The Consumer Product Safety Commission (CPSC) announced in a news release on Thursday, Dec. 4, that CreateOn’s Crayola-branded pip-cubes are being recalled after “posing an ingestion hazard to children.”
Around 9,400 units of the toy product are affected, according to the CPSC, as they contain magnetic building cubes “that can become loose if the seams separate.”
:max_bytes(150000):strip_icc():focal(940x1509:942x1511)/CreateOn-Recalls-Pip-Cubes-120625-05-b1346a5f24ff47b2998073c6cc37f8e5.jpg)
“When high-powered magnets are swallowed, the ingested magnets can attract to each other, or other metal objects, and become lodged in the digestive system,” the CPSC said.
This potential hazard can cause perforations, twisting or blockage of the intestines, blood poisoning and death, according to the organization.
The recalled pip-cube sets sold for around $20 at Michael’s Stores across the U.S. and online at Michaels.com and Amazon.com from May to July.
The affected products were sold in sets of 24 or 27 “Bold Colors” packs containing red, green, blue and yellow cubes, and “Glitter “packs containing purple, pink, blue and green cubes.
The brand name “Crayola” is imprinted on the left side of each cube. The model/UPC numbers of the recalled toys can be found on the bottom of the product packaging, according to the CPSC.
Consumers are being advised to “immediately stop using the recalled magnetic building cubes” and return the product using a pre-paid label provided by CreateOn. Replacement pip-cubes are also being offered.
Melinda
Reference:
Melinda
Another recall! Maybe it’s time to grow our own food and make everything from scratch.
Costco, which was among the impacted retailers, previously issued a warning in November
Thousands of cases of salad dressing have been recalled following concerns that a “foreign object” could be inside.
In a newly released exposure report from the Food and Drug Administration (FDA), the federal agency announced that 3,556 cases of various salad dressings from Ventura Foods had been affected in multiple states across the country.
The California-based company warned the public that “foreign objects (black plastic planting material) in granulated onion” might be found inside its products.
The alert was assigned a Class II label, which refers to “a situation in which use of, or exposure to, a violative product may cause temporary or medically reversible adverse health consequences or where the probability of serious adverse health consequences is remote.”
Impacted condiments include Creamy Poblano Avocado Ranch Dressing and Dip, Ventura Caesar Dressing, Pepper Mill Regal Caesar Dressing, Pepper Mill Creamy Caesar Dressing and Hidden Valley Buttermilk Ranch.
Two Caesar dressings specifically sold at Costco are also impacted.
“Costco and Ventura foods are announcing the recall of select Sell By dates of Item #19927 Caesar Salad and Item #11444 Chicken Sandwich w/ Caesar Salad due to the possible presence of plastic foreign material in the salad dressing of the items,” the brands said in a joint statement in November.
After sharing the “sell by” dates of the affected products, customers were urged to “Please stop eating the product and return the item to your local Costco for a full refund.”
In the most recent recall, the FDA said Ventura Foods had distributed the products to seven retail customers across 42 locations.
Affected states include: Arkansas, Colorado, Florida, Georgia, Illinois, Indiana, Kansas, Kentucky, Louisiana, Maryland, Michigan, Minnesota, Missouri, Nebraska, New Hampshire, New Jersey, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, South Carolina, Texas, Virginia, Washington and Wisconsin.
Melinda
Reference:
Melinda
Here are a few products my husband & I are using right now and a few main stays. I hope you find a product to add to your wellness routine. The list may also give you ideas for a surprise for friends, and family. Most products are found on Amazon however, I’m not an Amazon Affiliate and I make no commission from you using the links. Each link takes you directly to the items Amazon page.
Up to 12 Hours Temporary Relief of Mild to Moderate Pain, Backache, Sore Muscle, Sprains, Bruises. Clinically studied & effective to temporarily relieve mild to moderate pain.
Contains two powerful pain fighting ingredients, menthol and methyl salicylate (an NSAID – a nonsteroidal anti-inflammatory drug).
Rounded corners that resist peeling and flexible fabric.
Discreet and Comfortable: Thin, flexible design conforms to your body, making them suitable for use at home, work, or on the go.
Visit the Sleep Innovations Store
Featuring pressure-relieving TEMPUR-Material™ and our adjustable blend for the ideal balance of comfort and support. 5-Year Warranty, Adjustable fill for personalized sleep, and This item features a removable, machine-washable cover so you can refresh your sleep space as often as you like.
https://www.tempurpedic.com/shop-pillows/cloud-hybrid-pillow/v/4346/
For Body Muscle Pain Cramps Relief, 6 Heat Settings Machine Washable Electric Heating Pad. Soft Multi-Function Heating Pad: Heating pads for women are made of ultra-fine plush and can be used on double sides, It is extremely soft and gives you unexpected gentle care. Electric heating pad can achieve rapid heating within a few seconds, and provides overheating protection, auto shut off, timing and other safety protection functions, allowing you to enjoy the happiness of pain relief without worry
6 Heating Levels & 4 Timing Settings: Warmth and pain relief in one heating pad with 6 heating levels from 104℉(40℃) to 149℉ (65℃) and 4 timer settings (1h/2h/4h/6h). Whether it’s a mild to strong and lasting hot compress effect, or keeping warm in the cold winter, large heating pad can help you choose the most appropriate heating temperature and timer according to the degree of physical discomfort at any time
My husband and I can’t live without these products, they have improved our life and especially our sleeping.
Reference: