Are worries about tariffs, inflation, and the future of your 401(k) causing you to stress eat and lose sleep? Unfortunately, for most people, financial stress is nothing new.
“Studies have shown for decades that financial concerns are one of the leading causes of stress in our country, and until it is no longer a taboo topic, that’s not likely to change,” says Ashley Agnew, director of financial wellness and certified financial therapist at Centerpoint Advisors in Needham, Massachusetts.
Chronically high levels of anxiety about money can take a toll on your well-being, and even increase the likelihood of chronic illnesses like high blood pressure and heart disease.
All of this points to the importance of learning coping strategies that can help you manage financial stress and protect your mental and physical health.
When Financial Stress Becomes Toxic
“Normal financial stress tends to be situational; it’s often based on a specific event like moving or the holidays,” says Megan McCoy, PhD, associate professor at Kansas State and certified financial therapist in Manhattan.
If financial stress isn’t based around a specific event, and lasts more than three months, this may be a sign that your stress is turning into financial anxiety that may negatively impact your health, says Dr. McCoy.
According to McCoy, signs that could indicate severe or chronic financial stress include:
- Persistent worries, panic attacks, excessive rumination about bills or debts, and fear of checking bank balances — or going in the other direction, and compulsively checking bank or retirement balances
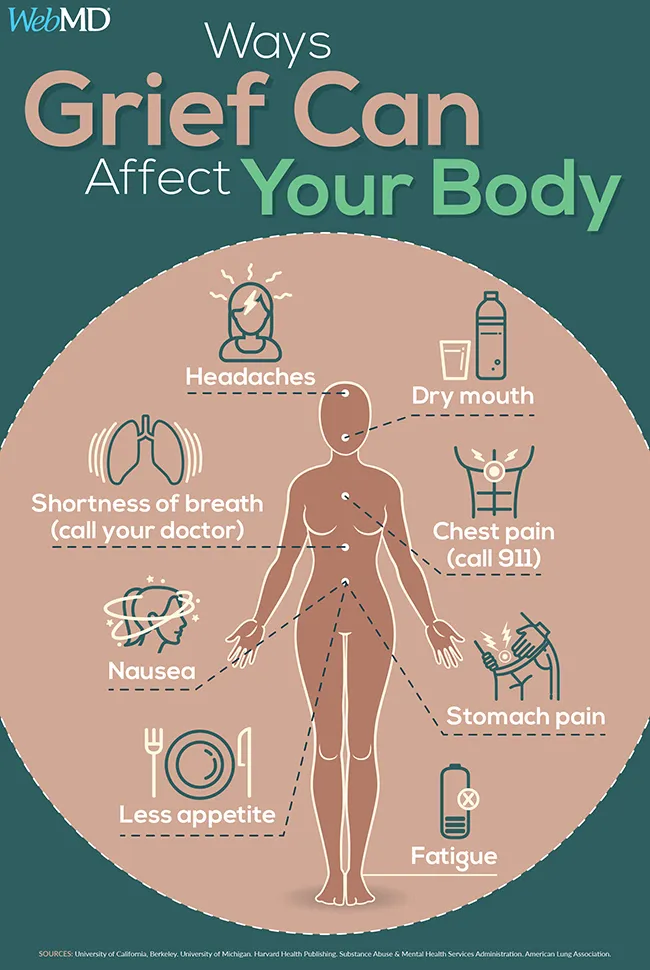
- Physical symptoms like recurrent headaches, stomachaches, or sleeping difficulties due to financial woes
- Avoiding looking at or paying bills
- Overusing alcohol and drugs to cope
- Overspending due to anxiety or hopelessness
- Relationship issues such as frequent arguments, withholding financial information from a partner, and lying about spending
How Financial Stress Impacts Your Health
Financial stress that’s gotten out of control can have health consequences.
Mental Health Issues
“People who have higher financial stress are at greater risk for anxiety disorders and clinical depression,” says McCoy.
Research suggests that financial strain — basically, the inability to cover expenses with available resources — is significantly associated with depression.
A review of 40 studies concluded that financial stress was linked with a greater likelihood of experiencing depression across all income levels, although this link was stronger for people with low incomes.
An online survey of over 1,600 adults found that 42 percent reported financially related panic or anxiety attacks. Younger generations such as Gen Zers and Millennials were particularly affected, with nearly half reporting these attacks — nearly double the rate found among Baby Boomers.
Shame and guilt can creep in due to financial stress, says McCoy. “Clients in financial therapy often describe feelings of unworthiness or guilt around unpaid debts or perceived poor financial decisions, making mental distress even worse,” she says.
A report on how financial stress impacts work found that worries about money caused a 34 percent increase in absenteeism and tardiness, and that financially stressed employees miss about twice as many work days each year compared with their non-financially-stressed counterparts.
Financial stress can also lead to negative coping behaviors, says McCoy. “Alcohol or drugs may be used to numb stress, creating dual crises — financial and addictive — that require integrated therapy approaches,” she says.
Sleep Problems
“People often report difficulty falling asleep or staying asleep when debts or bill payments weigh heavily on the mind,” says McCoy.
Experiencing financial strain is linked with insomnia, poor sleep quality, and not sleeping the recommended amount.
While a restless night here and there isn’t cause for concern, sleep issues that persist and become chronic can increase the likelihood of many chronic conditions, including dementia, heart disease, type 2 diabetes, and even cancers of the breast, colon, ovaries, and prostate.
Heart Disease and Other Chronic Illness
Stress triggers a series of physical reactions — your heart rate quickens, muscles tense, and breathing quickens — thanks to increased levels of the stress hormonescortisol and adrenaline (which act like messengers, readying the body to cope with a perceived threat).
If this response is chronic, as can be the case with financial stress, it can lead to problems like hypertension, high cholesterol, and muscle pain.
Research suggests that people who are frequently stressed about having enough money to pay their rent or mortgage have double the risk of heart disease compared with people who saw themselves as financially secure.
A review of five studies that looked at heart health outcomes found that people under financial stress had a 19 percent greater risk for heart disease or a major cardiac event like a stroke or heart attack.
Financial stress has also been linked to worse biological health as measured by inflammatory biomarkers. Researchers found that financial strain was “the most detrimental to biological health,” compared with other kinds of stress, including death of a loved one or divorce, although the study authors said that more research was needed to confirm this finding. They theorized financial stress was the hardest on the body because it can affect so many areas of life, “leading to family conflict, social exclusion, and even hunger or homelessness.”
And for people who already have chronic conditions or health issues, financial stress may exacerbate the problems. “When money is scarce, people are more likely to skip doctor visits, ignore recommended treatments, or fail to fill prescriptions,” says McCoy.
How to Cope With Financial Stress
There are ways to manage financial stress that don’t involve winning the lottery. Remember, financial wellness is about feeling secure about your money matters (even if funds are low) and not feeling overwhelmed to the point where it takes a toll on your health.
“Acknowledging the problem is essential — avoidance only heightens fear,” says McCoy.
With her clients, McCoy normalizes stress around money and finances by reminding clients that many people struggle with the same issues and that help is available. “This helps them move past shame to tangible action,” she says.
From a financial therapy standpoint, improvement usually takes both practical financial steps and attention to emotional/behavioral patterns. McCoy suggests a potential plan of attacking your financial fears:
Create a realistic budget or spending plan. Track income and expenses, prioritize needs, and set attainable goals, like saving to create a small emergency savings target.
“A values-based approach can help you align spending with personal or family values, making the process more meaningful and less punitive,” McCoy says.
Engage professional support. Work with a financial counselor or planner to help with debt management, savings strategies, and long-term planning.
These financial wellness specialists include certified credit counselors, accredited financial counselors (AFC), or financial therapists who are trained to integrate financial knowledge with mental health.
Leverage workplace or community resources. Employee Assistance Programs (EAPs) often provide free short-term counseling and financial education. Additionally, community nonprofits like cooperative extension offices or local credit unions may host free classes on budgeting or debt management.
Incorporate stress-management techniques. Consistent exercise, mindfulness, or journaling about money anxieties can help reduce the emotional intensity of financial worries.
Build an emergency savings fund a little at a time. Even $50 a month can accumulate into a basic safety net. Small, steady progress fosters a sense of accomplishment, which is key to reducing stress.
The Takeaway
- A certain amount of stress is normal, particularly when it is situational and related to a specific event.
- Chronic financial stress, however, can harm both mental and physical health, increasing the risk of anxiety, depression, sleep problems, and heart disease.
- While you can’t control all your financial stressors, you may be able to manage your response through realistic budgeting, professional support, and stress-reducing habits.
Resources We Trust
- Cleveland Clinic: Stress Management and Emotional Health
- Mayo Clinic: Chronic Stress Puts Your Health at Risk
- HelpGuide.org: Coping With Financial Stress
- Columbia University Irving Medical Center: The Link Between Health and FInancial Well-Being
- American Psychological Association: Money
Melinda
Reference: